Chapter: Clinical Dermatology: Infections
Viral infections: Herpes zoster
Herpes
zoster
Cause
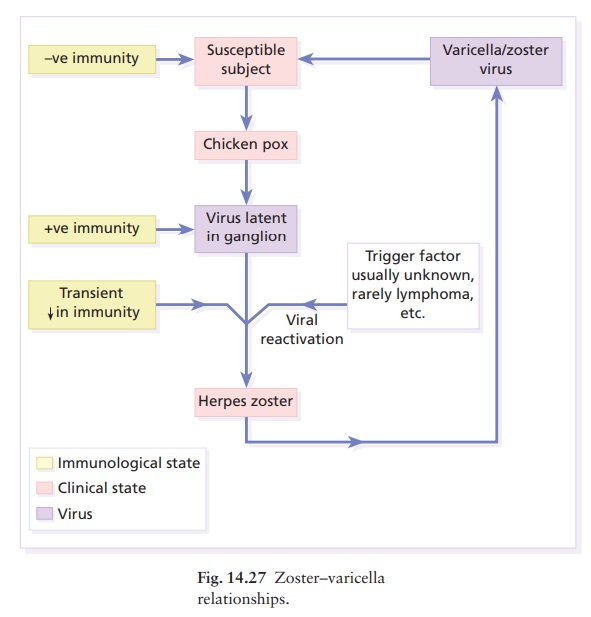
Shingles
too is caused by the herpes virus varicella-zoster. An attack is a result of
the reactivation, usually for no obvious reason, of virus that has remained
dormant in a sensory root ganglion since an earlier episode of chickenpox
(varicella). The incidence of shingles is highest in old age, and in conditions
such as HodgkinŌĆÖs disease, AIDS and leukaemia, which weaken normal defence
mechanisms. Shingles does not occur in epidemics; its clinical manifestations
are caused by virus acquired in the past. However, patients with zoster can
transmit the virus to others in whom it will cause chickenpox (Fig. 14.27).
Presentation and course
Attacks
usually start with a burning pain, soon followed by erythema and grouped,
sometimes blood-filled, vesicles scattered over a dermatome. The clear vesicles
quickly become purulent, and over the space of a few days burst and crust.
Scabs usually separate in 2ŌĆō3 weeks, sometimes leaving depressed depig-mented
scars.
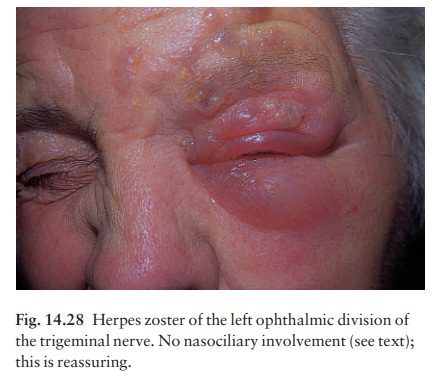
Zoster is characteristically unilateral (Fig. 14.28). It may affect more than one adjacent dermatome. The thoracic segments and the ophthalmic division of the trigeminal nerve are involved disproportionately often.
It
is not uncommon for a few pock-like lesions to be found outside the main
segment of involvement, but a generalized chickenpox-like eruption accompanying
segmental zoster should raise suspicions of an under-lying immunocompromised
state or malignancy, par-ticularly if the lesions are unusually haemorrhagic or
necrotic.
Complications
ŌĆó
Secondary bacterial infection is
common.
ŌĆó
Motor nerve involvement is uncommon,
but has led to paralysis of ocular muscles, the facial muscles, the diaphragm
and the bladder.
ŌĆó
Zoster of the ophthalmic division of
the trige-minal nerve can lead to corneal ulcers and scarring. A good clinical
clue here is involvement of the naso-ciliary branch (vesicles grouped on the
side of the nose).
ŌĆó
Persistent neuralgic pain, after the
acute episode is over, is most common in the elderly.
Differential diagnosis
Occasionally, before the rash has appeared, the initial pain is taken for an emergency such as acute appendicitis or myocardial infarction. Otherwise, the dermatomal distribution, and the pain, allow zoster to be distinguished easily from herpes simplex, eczema and impetigo.
Investigations
Cultures
are of little help as they take 5ŌĆō7 days, and are only positive in 70% of
cases. Biopsy or Tzanck smears show multinucleated giant cells and a ballooning
degeneration of keratinocytes, indicative of a herpes infection. Any clinical
suspicions about underlying conditions, such as HodgkinŌĆÖs disease, chronic
lymphatic leukaemia or AIDS, require further investigation.
Treatment
Systemic
treatment should be given to all patients if diagnosed in the early stages of
the disease. It is essen-tial that this treatment should start within the first
5 days of an attack. Famciclovir and valaciclovir are as effective as
aciclovir; they depend on virus-specific thymidine kinase for their antiviral
activity. All three drugs are safe, and using them may cut down the chance of
getting postherpetic neuralgia, particularly in the elderly.
If
diagnosed late in the course of the disease, systemic treatment is not likely
to be effective and treatment should be supportive with rest, analgesics and
bland applications such as calamine. Secondary bacterial infection should be
treated appropriately.
A
trial of systemic carbamazepine, gabapentin or amitriptyline, or 4 weeks of
topical capsaicin cream, despite the burning sensation it sometimes causes, may
be worthwhile for established post-herpetic neuralgia.
Cause
Herpesvirus
hominis is the cause of herpes simplex. The virus is ubiquitous and carriers
continue to shed virus particles in their saliva or tears. It has been
separated into two types. The lesions caused by type II virus occur mainly on
the genitals, while those of type I are usually extragenital; however, this
distinction is not absolute.
The
route of infection is through mucous mem-branes or abraded skin. After the
episode associated with the primary infection, the virus may become latent,
possibly within nerve ganglia, but still cap-able of giving rise to recurrent
bouts of vesication (recrudescences).
Presentation
Primary infection
The
most common recognizable manifestation of a primary type I infection in
children is an acute gin-givostomatitis accompanied by malaise, headache, fever
and enlarged cervical nodes. Vesicles, soon turn-ing into ulcers, can be seen
scattered over the lips and mucous membranes. The illness lasts about 2 weeks.
Primary
type II virus infections, usually transmitted sexually, cause multiple and
painful genital or peri-anal blisters which rapidly ulcerate.
The
virus can also be inoculated directly into the skin (e.g. during wrestling). A
herpetic whitlow is one example of this direct inoculation. The uncom-fortable
pus-filled blisters on a fingertip are seen most often in medical personnel
attending patients with unsuspected herpes simplex infections.
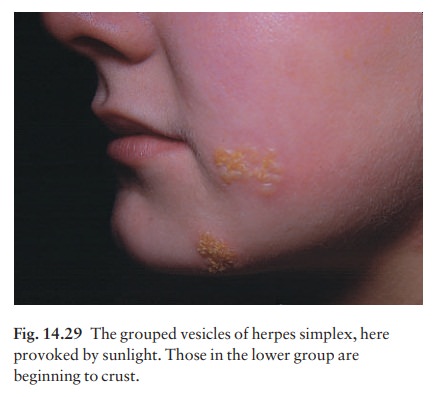
Recurrent (recrudescent) infections
These strike in roughly the same place each time. They may be precipitated by respiratory tract infections (cold sores), ultraviolet radiation, menstruation or even stress. Common sites include the face (Fig. 14.29) and lips (type I), and the genitals (type II), but lesions can occur anywhere. Tingling, burning or even pain is followed within a few hours by the development of erythema and clusters of tense vesicles. Crusting occurs within 24 ŌĆō 48 h and the whole episode lasts about 12 days.
Complications
ŌĆó
Herpes encephalitis or meningitis
can occur with-out any cutaneous clues.
ŌĆó
Disseminated herpes simplex:
widespread vesicles may be part of a severe illness in newborns, debilitated
children or immunosuppressed adults.
ŌĆó
Eczema herpeticum: patients with
atopic eczema are particularly susceptible to widespread cutaneous herpes
simplex infections. Those looking after patients with atopic eczema should stay
away if they have cold sores.
ŌĆó
Herpes simplex can cause recurrent
dendritic ulcers leading to corneal scarring.
ŌĆó
In some patients, recurrent herpes
simplex infections are regularly followed by erythema multiforme.
Investigations
None
are usually needed. Doubts over the diagnosis can be dispelled by culturing the
virus from vesicle fluid. Antibody titres rise with primary, but not with
recurrent infections.
Treatment
ŌĆśOld-fashionedŌĆÖ
remedies suffice for occasional mild recurrent attacks; sun block may cut down
their frequency. Dabbing with surgical spirit is helpful, and secondary
bacterial infection can be reduced by topical bacitracin, mupirocin, framycetin
or fusidic acid. For more severe and frequent attacks, aciclovir cream, if used
at the first sign of the recrudescence, and applied five or six times a day for
the first 4 days of the episode, cuts down the length of attacks and perhaps
increases the intervals between them.
Aciclovir
tablets, 200 mg five times daily for 5 days, is more effective and can be given
to those with widespread or systemic involve-ment. Recurrences in the
immunocompromised can usually be prevented by long-term treatment at a lower
dosage. Famciclovir and valaciclovir are meta-bolized by the body into
aciclovir and are as effective as aciclovir, having the additional advantage of
need-ing fewer doses per day.
Related Topics