Chapter: Ophthalmology: Retina
Retinal Arterial Occlusion
Retinal Arterial Occlusion
Definition
Retinal infarction due to occlusion of an artery in the lamina cribrosa or a branch retinal artery occlusion.
Epidemiology:
Retinal artery occlusions occur significantly less often
thanvein occlusions.
Etiology:
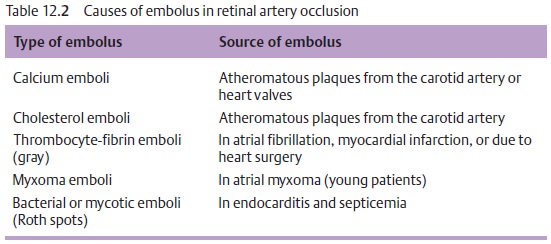
Emboli (Table 12.2) arefrequentlythe cause of retinal artery andbranch retinal artery occlusions. Less frequent causes include inflammatory processes such as temporal arteritis (Horton’s arteritis).
Horton’s arteritis should be excluded where
retinal artery occlusion is accompanied by headache.
Symptoms:
Incentral retinal artery
occlusion, the patient generally com-
plains of sudden,
painless unilateral blindness. In branch retinal artery occlu-sion, the patient will notice a loss of visual acuity or visual
field defects.
Diagnostic considerations:
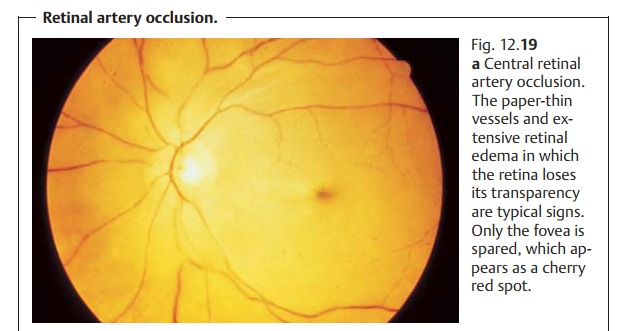
The diagnosis is made by ophthalmoscopy. Inthe acute stage of central retinal artery
occlusion, the retina appears grayishwhite due to edema of the layer
of optic nerve fibers and is no longer
trans-parent. Only the fovea
centralis, which contains no nerve fibers, remains vis-ible as a “cherry red spot” because the red of the
choroid shows through at this site (Fig. 12.19a). The column of blood will be seen to be interrupted. Rarely
one will observe an embolus. Patients with a cilioretinal artery (artery
origi-nating from the ciliary arteries instead of the central retinal artery)
will exhibit normal perfusion in the area of vascular supply, and their loss of
visual acuity will be less. Atrophy of
the optic nerve will develop in the chronic
stageof central retinal artery occlusion.
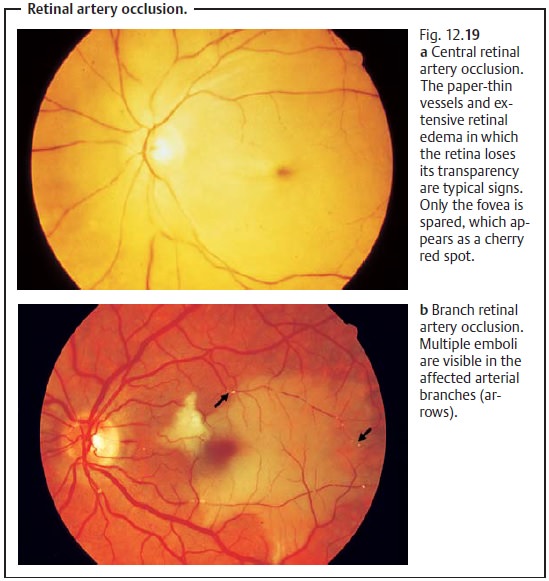
In the acute stage of central retinal artery
occlusion, the fovea centralis appears as cherry red spot on ophthalmoscopy.
There is not edema of the layer of optic nerve fibers in this area because the
fovea contains no nerve fibers.
In branch retinal artery occlusion, a retinal edema will be found in the
affected area of vascular supply (Fig. 12.19b). Perimetry (visual field testing) will reveal a total visual field defect
in central retinal artery occlusion and a partial defect in branch occlusion.
Differential diagnosis:
Lipid-storage diseases that can also create a cherryred spot such as Tay-Sachs disease, Niemann-Pick disease, or Gaucher’s dis-ease should be excluded. These diseases can be clearly identified on the basis of their numerous additional symptoms and the fact that they afflict younger patients.
Treatment:
Emergency treatment is often unsuccessful even when
initiatedimmediately. Ocular massage, medications that reduce intraocular
pressure, or paracentesis are applied in an attempt to drain the embolus in a
peripheral retinal vessel. Calcium antagonists or hemodilution are applied in
an attempt to improve vascular supply. Lysis therapy is no longer performed due
to the poor prognosis (it is not able to prevent blindness) and the risk to
vital tissue involved.
Prophylaxis:
Excluding or initiating prompt therapy of predisposing
under-lying systemic disorders is crucial (see Table 12.2).
Clinical course and prognosis:
The prognosis is poor becauseirreparabledamage
to the inner layers of the retina occurs
within one hour. Blindness usu-ally cannot be prevented in central retinal
artery occlusion. The prognosis is better where only a branch of the artery is
occluded unless a macular branch is affected.
Related Topics