Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Peripheral Nerve Blocks
Upper Extremity Peripheral Nerve Blocks: Supraclavicular Block
Supraclavicular Block
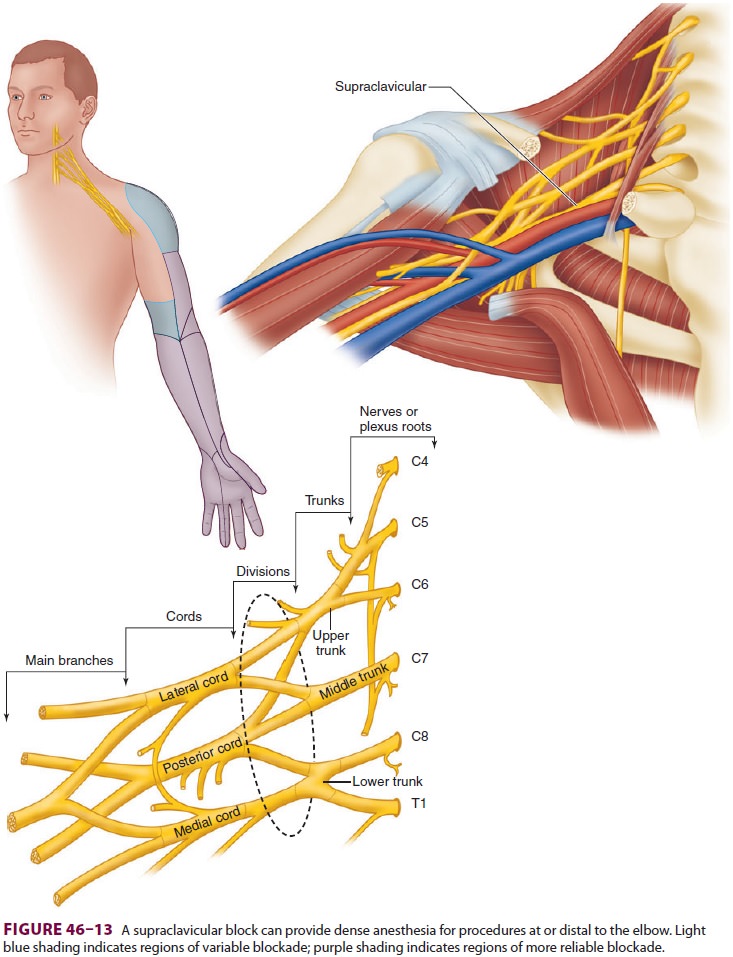
Once described as the “spinal of the arm,” a supra-clavicular block
offers dense anesthesia of the brachial plexus for surgical procedures at or
dis-tal to the elbow (Figure 46–13). Historically, the
supraclavicular block fell out of favor due to the high incidence of
complications (namely, pneumo-thorax) that occurred with paresthesia and nerve
stimulator techniques. It has seen a resurgence in recent years as the use of
ultrasound guidance has theoretically improved safety. The supraclavicu-lar
block does not reliably anesthetize the axillary and suprascapular nerves, and
thus is not ideal for shoulder surgery. Sparing of distal branches,
par-ticularly the ulnar nerve, may occur. Supraclavicu-lar perineural catheters
provide inferior analgesia compared with infraclavicular infusion and are often
displaced due to a lack of muscle mass to aid catheter retention.
Many of the same precautions that are taken with patient selection for
an interscalene block should be exercised with a supraclavicular block. Nearly
half of patients undergoing supraclavicu-lar block will experience ipsilateral
phrenic nerve palsy, although this incidence may be decreased by using
ultrasound guidance, allowing use of a mini-mal volume of local anesthetic.
Horner’s syndrome and recurrent laryngeal nerve palsy may also occur. Pneumothorax
and subclavian artery puncture, although theoretically less likely under
ultrasound guidance, remain potential risks.
A. Ultrasound
The patient should be supine with the head
turned 30o
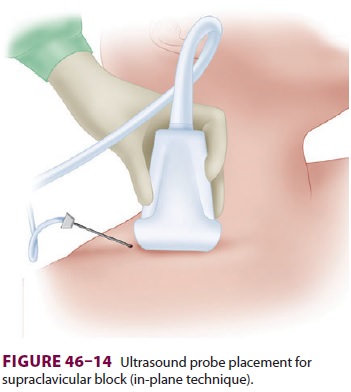
toward the contralateral side. A linear, high-frequency transducer is placed in
the supraclavicu-lar fossa superior to the clavicle and angled slightly toward
the thorax (Figure 46–14). The subclavian artery
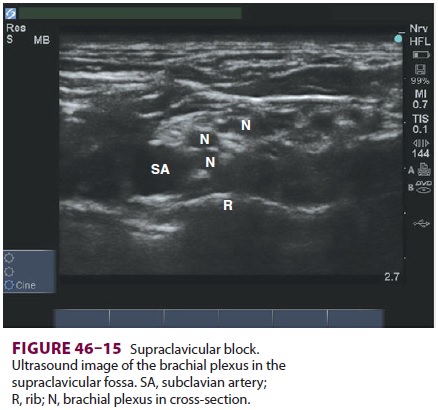
should be easily identified. The brachial plexus appears as multiple hypoechoic
disks just superficial and lateral to the subclavian artery (Figure
46–15). The first rib should also be identified as
a hyperechoic line just deep to the artery. Pleura may be identified adjacent
to the rib, and can be distinguished from bone by its movement with breathing.
For an out-of-plane technique, a short,
22-gauge blunt-tipped needle is used. The skin is anesthe-tized, and the needle
inserted just cephalad to the ultrasound transducer in a posterior and caudad
direction. After careful aspiration for the nonap-pearance of blood,
30–40 mL of local anesthetic s injected in 5-mL increments while visualizing
local anesthetic spread around the brachial plexus.
For an in-plane technique, a longer needle may be necessary. The needle is inserted lateral to the transducer in a direction parallel to the ultrasound beam. The needle is advanced medially toward the subclavian artery until the tip is visualized near the brachial plexus just lateral and superficial to the artery. Local anesthetic spread should be visualized surrounding the plexus after careful aspiration and incremental injection, which often requires injec-tions in multiple locations and a highly variable vol-ume (20–30 mL).
Related Topics