Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Peripheral Nerve Blocks
Upper Extremity Peripheral Nerve Blocks: Infraclavicular Block
Infraclavicular Block
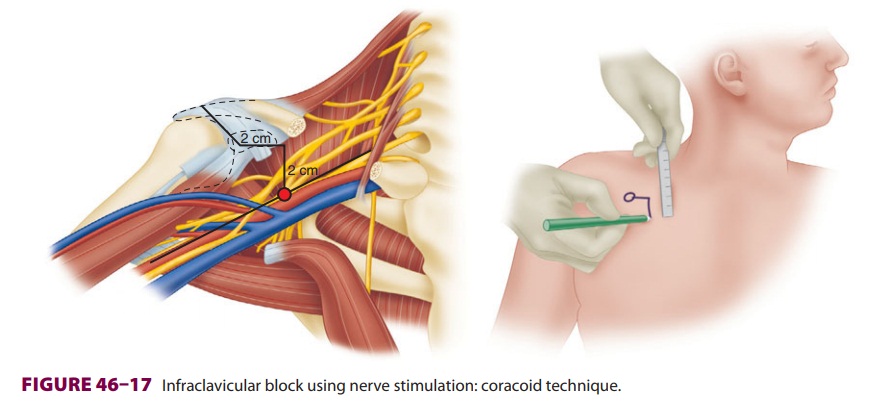
Brachial plexus block at the level of the
cords provides excellent anesthesia for procedures at or distal to the elbow ( Figure
46–16). The upper arm and shoulder are not
anesthetized with this approach. As with other brachial plexus blocks, the
intercostobrachial nerve (T2 derma-tome) is spared. Site-specific risks of the
infracla-vicular approach include vascular puncture and pneumothorax (although
less common than with supraclavicular block). It is often prudent to avoid this
approach in patients with vascular catheters in the subclavian region, or
patients with an ipsilat-eral pacemaker.
As the brachial plexus traverses beyond the
first rib and into the axilla, the cords are arranged around the axillary
artery according to their anatomic posi-tion: medial, lateral, and posterior.
A. Nerve Stimulation
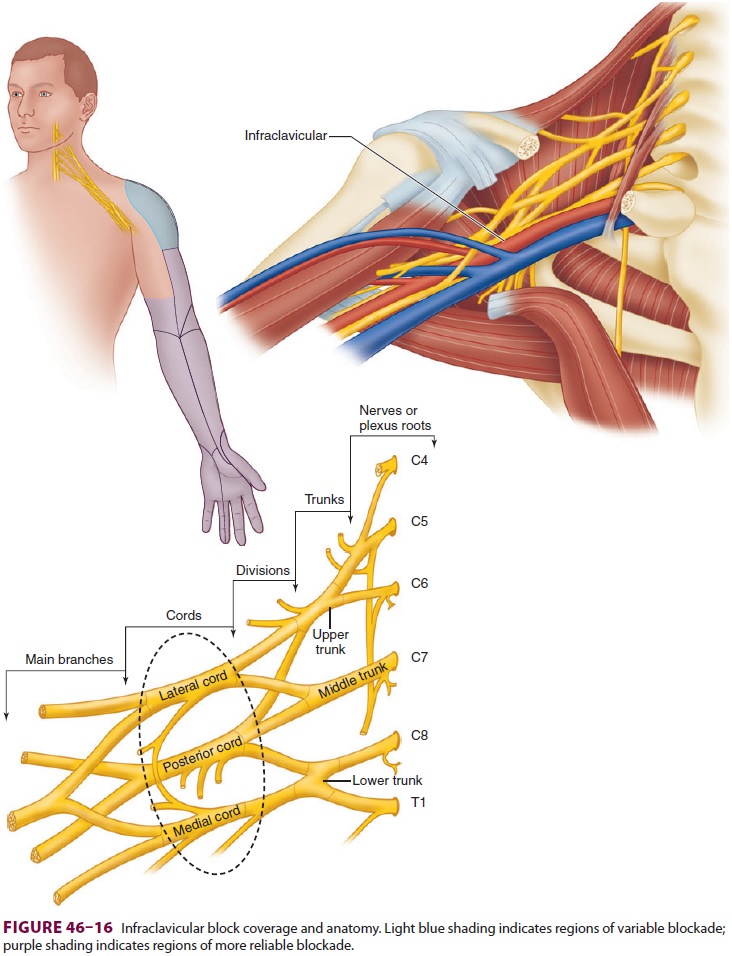
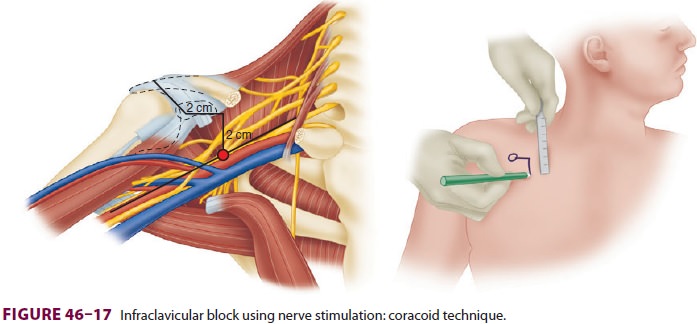
The patient is positioned supine with the
head turned to the contralateral side, and the coracoid process is identified
(a bony prominence of the scapula that can be palpated between the
acromioclavicular joint and the deltopectoral groove). The subclavian artery
and brachial plexus run deep to the cora-coid process and can be found
approximately 2 cm medial and 2 cm caudad to it, about 4–5 cm deep in the
average patient ( Figure 46–17).
A relatively long (8 cm) insulated needle is placed perpendicu-lar to the skin
and advanced directly posterior until a motor response is elicited. An
acceptable motor response is finger flexion or extension at a current less than
0.5 mA, but not elbow flexion/extension.
B. Ultrasound
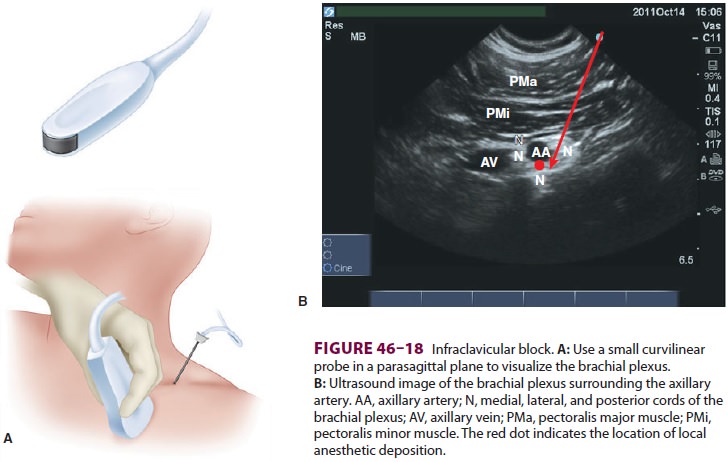
With the patient in the supine position, a small curvilinear transducer
is placed in the parasag-ittal plane over the point 2 cm medial and 2 cm caudad
to the coracoid process (Figure 46–18A). (Abducting the arm 90 o improves
axillary artery imaging.) A high-frequency linear transducer will often provide
inadequate needle visualization due to the relatively acute
needle-to-transducer angle. The axillary artery and vein are identified in
cross-section (Figure 46–18B). The medial, lateral, and posterior
cords appear as hyperechoic bundles posi-tioned caudad, cephalad, and posterior
to the artery, respectively. A relatively long needle is inserted 2–3 cm
cephalad to the transducer. Optimal needle positioning is between the axillary
artery and the posterior cord. Three randomized, controlled trials have
demonstrated equivalent results with a single 30-mL injection adjacent to the
posterior cord or divided among each of the cords. Insertion of a perineural
catheter should always be in the same location posterior to the axillary
artery, and infra-clavicular infusion has been shown to provide supe-rior
analgesia to both supraclavicular and axillary catheters.
Related Topics