Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Peripheral Nerve Blocks
Upper Extremity Peripheral Nerve Blocks: Axillary Block
Axillary Block
At the lateral border of the pectoralis minor
muscle, the cords of the brachial plexus form large terminalbranches.
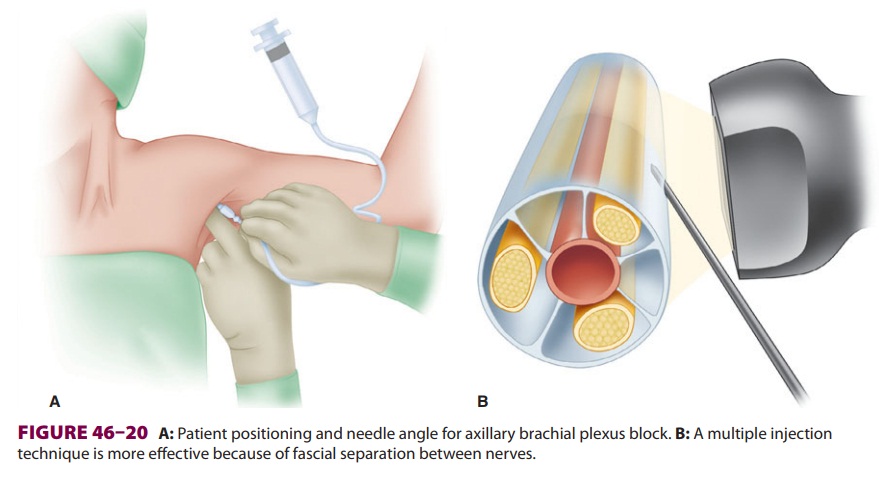
The axillary, musculocutaneous, and medial brachial cutaneous nerves branchfrom the
brachial plexus proximal to the location in which local anesthetic is deposited
during an axil-lary nerve block, and thus are usually spared (Figure
46–19). At this level, the major terminal nerves often are separated by
fascia; therefore mul-tiple injections (10-mL each) may be required to reliably
produce anesthesia of the entire arm distal to the elbow (Figure
46–20).
There are few contraindications to axillary
bra-chial plexus blocks. Local infection, neuropathy, and bleeding risk must be
considered. Because the axilla is highly vascularized, there is a risk of local
anes-thetic uptake through small veins traumatized by needle placement. The
axilla is also a suboptimal site for perineural catheter placement because of
greatly inferior analgesia versus an infraclavicular infusion, as well as
theoretically increased risks of infection and catheter dislodgement.
All of the numerous axillary block techniques
require the patient to be positioned supine, with the arm abducted 90 o and the head turned toward the contralateral
side (Figure 46–20). The axillary artery pulse should be palpated and its
location marked as a reference point.
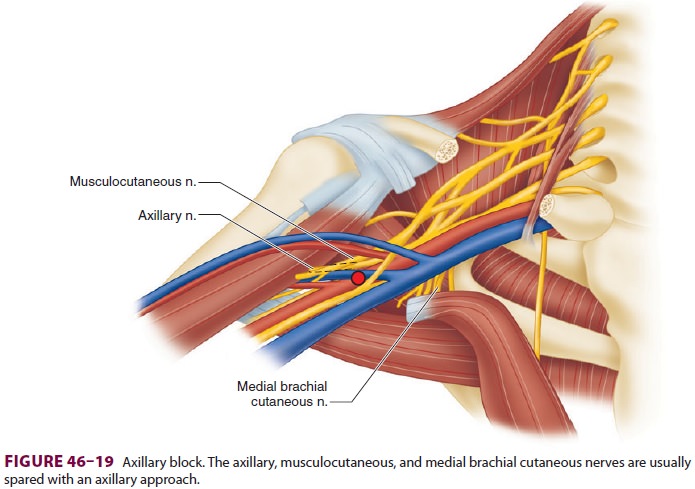
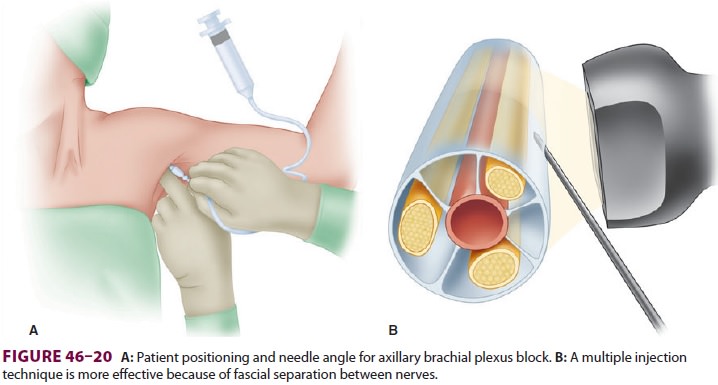
A. Transarterial Technique
This technique has fallen out of favor due to the trauma of twice
purposefully penetrating the axil-lary artery along with a theoretically
increased risk of inadvertent intravascular local anesthetic injec-tion. The
nondominant hand is used to palpate and immobilize the axillary artery, and a
22-gauge needle is inserted high in the axilla (Figure 46–20) until bright red blood
is aspirated. The needle is then slightly advanced until blood aspiration
ceases. Injection can be performed posteriorly, anteriorly, or in both
locations in relation to the artery. A total of 30–40 mL of local anesthetic is
typically used.
B. Nerve Stimulation
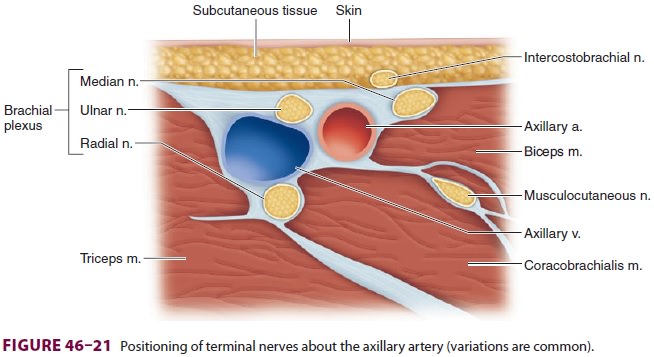
Again the nondominant hand is used to palpate
and immobilize the axillary artery. With the arm abducted and externally
rotated, the terminal nerves usually lie in the following positions relative to
the artery (Figure 46–21, although variations
are common): median nerve superior (wrist flexion, thumb opposition, forearm
pronation); ulnar nerve inferior (wrist flexion, thumb adduction, fourth/ fifth
digit flexion); and radial nerve inferior–poste-rior (digit/wrist/elbow
extension, forearm supina-tion). The musculocutaneous nerve (elbow flexion) is
separate and deep within the coracobrachialis muscle, which is more superior
(lateral) in this posi-tion and, as a consequence, is often not blocked with
this procedure (Figure 46–21). A 2-in., 22-gauge insulated needle is inserted
proximal to the palpat-ing fingers to elicit muscle twitches in the hand. Once
an acceptable muscle response is identified, and after reducing the stimulation
to less than 0.5 mA, careful aspiration is performed and local anes-thetic is
injected. Although a single injection of 40 mL may be used, greater success
will be seen with multiple nerve stimulations (ie, two or three nerves) and
divided doses of local anesthetic.
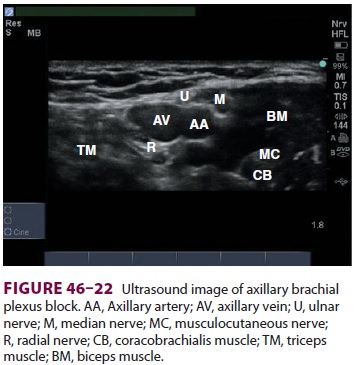
C. Ultrasound
Using a high-frequency linear array
ultrasound transducer, the axillary artery and vein are visual-ized in
cross-section. The brachial plexus can be identified surrounding the artery (Figure
46–22). The needle is inserted superior (lateral)
to the trans-ducer and advanced inferiorly (medially) toward the plexus under
direct visualization. Ten milliliters of local anesthetic is then injected
around each nerve (including the musculocutaneous, if indicated).
Related Topics