Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Peripheral Nerve Blocks
Lower Extremity Peripheral Nerve Blocks: Sciatic Nerve Block
Sciatic Nerve Block
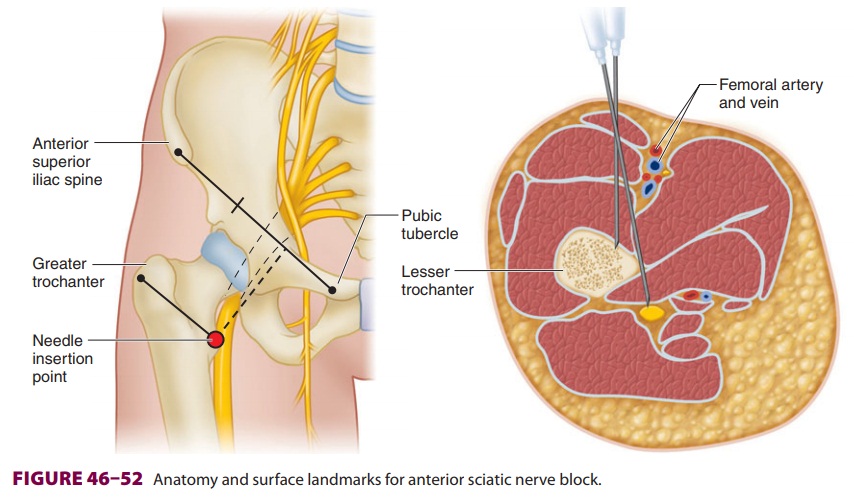
The sciatic nerve originates from the
lumbosacral trunk and is composed of nerve roots L4–5 and S1–3(see Figure
46–38). Blockade of the sciatic nerve may
occur anywhere along its courseand is indicated for surgical procedures
involving the hip, thigh, knee, lower leg, and foot. The poste-rior femoral
cutaneous nerve is variably anesthe-tized as well, depending on the approach.
If sacral plexus or posterior femoral cutaneous nerve anes-thesia is required,
the parasacral approach is used.
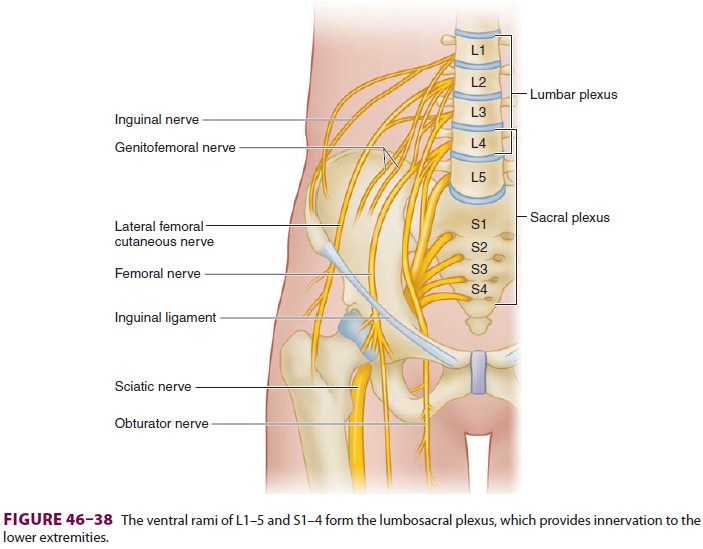
A. Posterior (Classic or Labat) Approach
The patient is positioned laterally with the
side to be blocked in the nondependent position. The patient is asked to bend
the knee of the affected leg and tilt the pelvis slightly forward (Sim’s
position; Figure 46–51). The greater
trochanter, posteriorsuperior iliac spine (PSIS), and sacral hiatus are then
identified. A line is drawn from the greater trochan-ter to the PSIS, its
midpoint identified, and a per-pendicular line extended in a caudal direction.
Next, a line is drawn from the greater trochanter to the
sacral hiatus and the intersection point is marked; this is the initial
needle insertion point. A long (10-cm) insulated needle is inserted at an angle
per-pendicular to all planes to the skin (Figure 46–51). The needle is advanced
through the gluteal muscles (a motor response of these muscles may be
encoun-tered) until plantar- or dorsiflexion is elicited (plan-tarflexion or
foot inversion is preferred for surgical anesthesia). A local anesthetic volume
of 25 mL pro-vides surgical anesthesia.
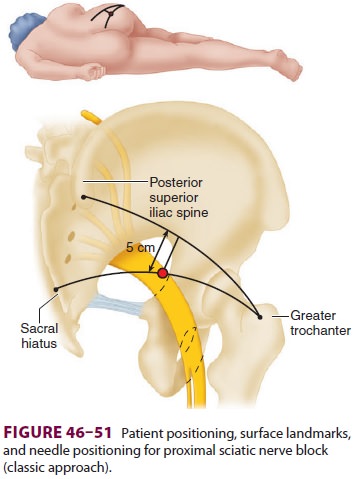
B. Anterior Approach
After leaving the sciatic notch, the sciatic
nerve descends behind the lesser trochanter to a position posterior to the
femur. It can be accessed from the anterior thigh just medial to the lesser
trochanter. Lateral or prone positioning may present a challenge for some
patients requiring a sciatic nerve block (ie, elderly patients, pediatric
patients under general anesthesia). An anterior approach can be technically
challenging but offers an alternative path to the sci-atic nerve. Before
proceeding with this block, which carries a risk of vascular puncture (femoral
artery and vein), patient-specific risks should be consid-ered (eg,
coagulopathy and vascular grafting). In addition, if combining this block with
the femoral nerve block in an unanesthetized patient, perform-ing the sciatic
block first is recommended to avoid passing the block needle through a
previously anes-thetized femoral nerve. A local anesthetic volume of 25 mL
provides surgical anesthesia.
Nerve stimulation—With the patient positionedsupine, a line is drawn along the inguinal
ligament, from the anterior superior iliac spine to the pubic tubercle (Figure
46–52). A second line is drawn par-allel to the
first that traverses the greater trochanter (intertrochanteric line). Next,
these two lines are connected with a third line drawn from the point between
the medial one third and lateral two thirds of the first line, at a 90° angle,
and extended caudally to intersect with the intertrochanteric line. A long (10-
to 15-cm) needle is inserted through this inter-section and directly posterior
until foot inversion or plantarflexion is elicited (dorsiflexion is accept-able
for postoperative analgesia). Often with this approach, the femur is contacted
before the needle reaches the sciatic nerve. When this occurs, the nee-dle
should be withdrawn 2–3 cm, the patient should be asked to internally rotate
the leg, and then the needle should be advanced. If the femur is contacted
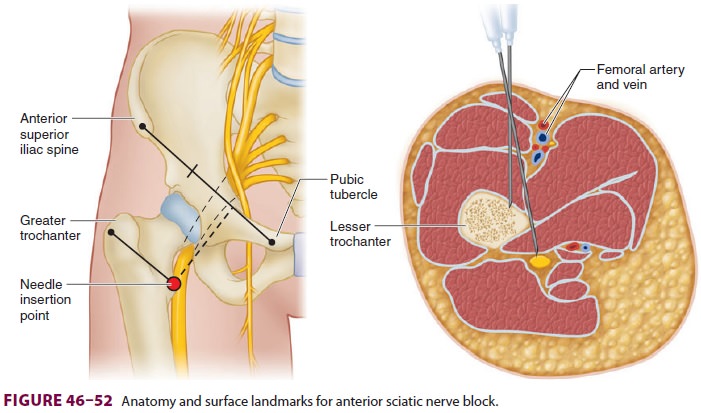
again, the landmarks may require reassessment. A local anesthetic volume
of 25 mL provides surgical anesthesia.
2. Ultrasound—With the patient positioned supineand the leg externally rotated, a
low-frequency cur-vilinear transducer is placed transversely over the medial
thigh, approximately at the level of the lesser trochanter. The femur, femoral
vessels, adductor muscles, and gluteus maximus are identified in cross-section.
The elliptical, hyperechoic sciatic nerve is found in the fascial plane between
adductors and gluteus muscles, posterior to the femur. Using a long (10-cm)
needle, the nerve is approached in-plane (anterior to posterior) or
out-of-plane (cephalad to caudad), taking care to avoid femoral vessels, until
the needle tip lies in this muscle plane and a local anesthetic injection can
be observed as hypoechoic spread surrounding the sciatic nerve.
C. Subgluteal Approach
A subgluteal approach to the sciatic nerve is
a useful alternative to the traditional posterior approach. In many patients
the landmarks are more easily iden-tified, and less tissue is traversed. With
the sciatic nerve at a more superficial location, the exclusive use of
ultrasound becomes far more practical, as well. If sciatic nerve block is being
combined with a femoral block and ambulation is desired within the local
anesthetic duration, consider a popliteal approach (below) that will not affect
the hamstring muscles to the same degree, allowing knee flexion to lift the
foot with the use of crutches.
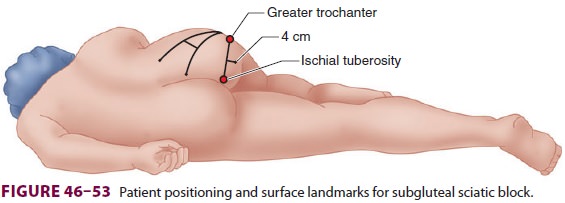
1. Nerve
stimulation—With the patient inSim’s position, the greater trochanter and
ischialtuberosity are identified and a line drawn between them (Figure
46–53). From the midpoint of this line, a second line is drawn
perpendicularly and extended caudally 4 cm. Through this point a long (10-cm)
insulated needle is inserted directly slightly cephalad until foot
plantarflexion or inversion is elicited (dorsiflexion is acceptable for
analgesia). A local anesthetic volume of 25 mL provides surgical anesthesia.
2.
Ultrasound—Using the same positioning andlandmarks (Figure 46–53), a linear or
low-frequency curvilinear (best) ultrasound transducer is placed over the
midpoint between the ischial tuberosity and the greater trochanter in a
transverse orienta-tion. Both bony structures should be visible in the
ultrasound field simultaneously. Gluteal muscles are identified superficially,
along with the fascial layer defining their deep border. The triangular sciatic
nerve should be visible in cross-section just deep to this layer in a location
approximately mid-way between the ischial tuberosity and the greater
trochanter, superficial to the quadratus femoris muscle.
For an out-of-plane ultrasound-guided sciatic block, the block needle is
inserted just caudad to the ultrasound transducer and advanced in an ante-rior
and cephalad direction. Once the needle passes through the gluteus muscles with
the tip next to sciatic nerve, careful aspiration for the nonappear-ance of
blood is performed and local anesthetic is injected, visualizing spread around
the nerve.
For an in-plane technique, the block needle is inserted just lateral to the ultrasound transducer near the greater trochanter. It is advanced through the field of the ultrasound beam until the tip is vis-ible deep to the gluteus maximus, next to the sci-atic nerve. Again, local anesthetic spread around the nerve should be visualized.
D. Popliteal Approach
Popliteal nerve blocks provide excellent
cover-age for foot and ankle surgery, while sparingmuch of the hamstring
muscles, allowing lifting of the foot with knee flexion, thus easing
ambulation. All sciatic nerve blocks fail to provide complete anesthesia for
the cutaneous medial leg and ankle joint capsule, but when a saphenous (or
femoral) block is added, complete anesthesia below the knee is provided. The
major site-specific risk of a popliteal block is vascular puncture, owing to
the sciatic nerve’s proximity to the popliteal vessels at this location.
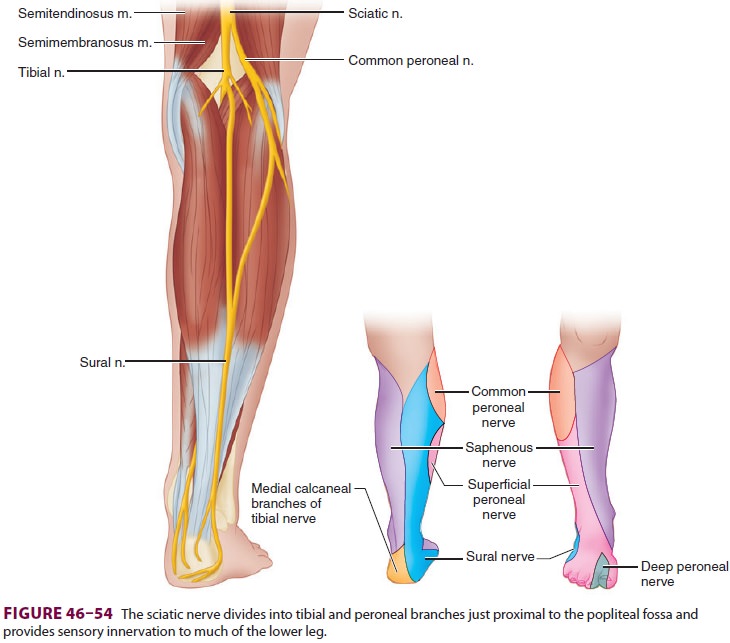
The sciatic nerve divides into the tibial and
common peroneal nerves within or just proximal to the popliteal fossa (Figure
46–54). The upper pop-liteal fossa is bounded
laterally by the biceps femo-ris tendon and medially by the semitendinosus and
semimembranosus tendons. Cephalad to the flexion crease of the knee, the
popliteal artery is immedi-ately lateral to the semitendinosus tendon. The
pop-liteal vein is lateral to the artery, and the tibial andcommon peroneal
nerves are just lateral to the vein and medial to the biceps tendon, 2–6 cm
deep to the skin. The tibial nerve continues deep behind the gastrocnemius
muscle, and the common peroneal nerve leaves the popliteal fossa by passing
between the head and neck of the fibula to supply the lower leg. The sciatic
nerve is approached by either a poste-rior or a lateral approach. For posterior
approaches, the patient is usually positioned prone with the knee slightly
flexed by propping the ankle on pillows or towels. For lateral approaches, the
patient may be in the lateral or supine position.
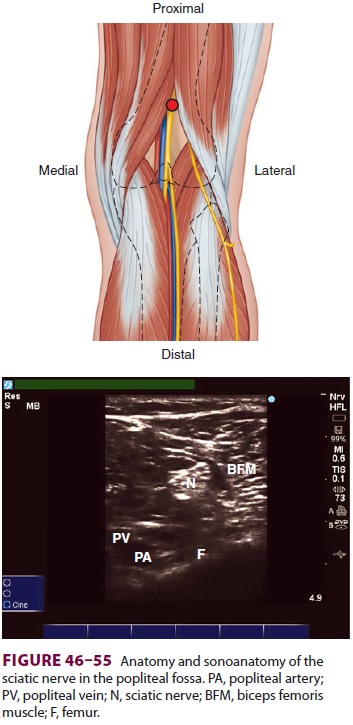
Nerve stimulation (posterior
approach)—Withthe patient in the prone position, the
apex of the popliteal fossa is identified. The hamstring muscles are palpated
to locate the point where the biceps femoris (lateral) and the
semimembranosus/semi-tendinosus complex (medial) join (Figure
46–55). Having the patient flex the knee against
resistance facilitates recognition of these structures. The nee-dle entry point
is 1 cm caudad from the apex. An insulated needle (5–10 cm) is advanced until
foot plantarflexion or inversion is elicited (dorsiflexion is acceptable for
analgesia). A volume of 30–40 mL of local anesthetic is often required for
single-injection popliteal–sciatic nerve block.
Nerve
stimulation (lateral approach)—Withthe patient in the supine
position and the knee fully extended, the intertendinous groove is palpated
between the vastus lateralis and biceps femoris muscles approximately 10 cm
proximal to the supe-rior notch of the patella. A long (10-cm) insulated needle
is inserted at this point and advanced at a 30° angle posteriorly until an
appropriate motor response is elicited. If bone (femur) is contacted, the
needle is withdrawn and redirected slightly posteriorly until an acceptable
motor response is encountered.
Ultrasound—With the patient positionedprone, the
apex of the popliteal fossa is identified, as described above. Using a
high-frequency linear ultrasound transducer placed in a transverse
orien-tation, the femur, biceps femoris muscle, popliteal vessels, and sciatic
nerve or branches are identi-fied in cross-section (Figure 46–55). The nerve is
usually posterior and lateral (or immediately pos-terior) to the vessels and is
often located in close
relationship to the biceps femoris muscle, just deep to its medial edge.
For an out-of-plane technique, the needle is
inserted just caudad to the ultrasound transducer and directed anteriorly and
slightly cephalad. When the needle is positioned in proximity to the sciatic
nerve, and following careful aspiration, local anesthetic injected, observing
for spread around the nerve.
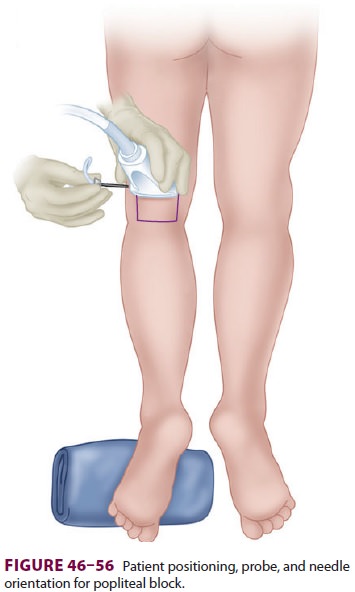
For an in-plane technique, the block needle is inserted lateral to the
ultrasound transducer, traversing—or just anterior to—the biceps femoris muscle
(Figure 46–56). The needle is advanced in the
ultrasound plane, while visualizing its approach either deep or superficial to
the nerve.
If surgical anesthesia is desired, local anesthetic should be seen
surrounding all sides of the nerve, which usually requires multiple needle tip
place-ments with incremental injection. For analgesia alone, a single injection
of local anesthetic is accept-able. Ultrasound-guided popliteal sciatic blocks
may be performed with the patient in the lateral or supine positions (the
latter with leg up-raised on several pillows). These maneuvers are often more
technically challenging.
Related Topics