Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Peripheral Nerve Blocks
Upper Extremity Peripheral Nerve Blocks: Interscalene Block
Interscalene Block
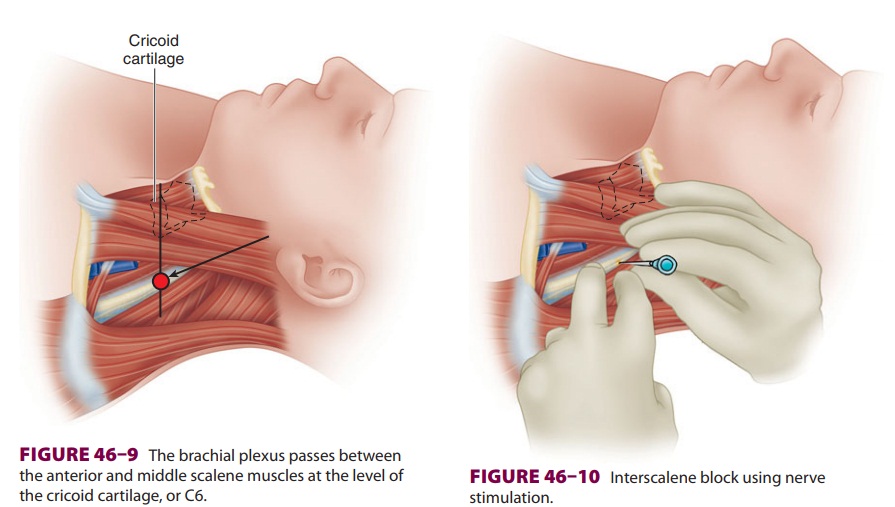
An interscalene brachial plexus block is
indicated for procedures involving the shoulder and upper arm (Figure
46–8). Roots C5–7 are most densely blocked with
this approach; and the ulnar nerve originating from C8 and T1 may be spared.
There-fore, interscalene blocks are not appropriate for sur-gery at or distal to
the elbow. For complete surgical anesthesia of the shoulder, the C3 and C4
cutane-ous branches may need to be supplemented with a superficial cervical
plexus block or local infiltration.Contraindications to an interscalene block
include local infection, severe coagulopathy, local anesthetic
allergy, and patient refusal. A properly
performed interscalene block invariably blocks the ipsilateral phrenic nerve
(completely for nerve stimulation techniques; unclear for ultra-sound-guided
techniques), so careful consideration should be given to patients with severe
pulmonary disease or preexisting contralateral phrenic nerve palsy. The
hemidiaphragmatic paresis may result in
dyspnea, hypercapnia, and hypoxemia. A Horner’s syndrome (myosis,
ptosis, and anhidrosis) may result from proximal tracking of local anesthetic
and blockade of sympathetic fibers to the cervico-thoracic ganglion. Recurrent
laryngeal nerve involvement often induces hoarseness. In a patient with contralateral
vocal cord paralysis, respiratory distress may ensue. Other site-specific risks
include vertebral artery injection (suspect if immediate sei-zure activity is
observed), spinal or epidural injec-tion, and pneumothorax. Even 1 mL of local
anesthetic delivered into the vertebral artery may induce a seizure. Similarly,
intrathecal, subdural, and epidural local anesthetic spread is possible.Lastly,
pneumothorax is possible due to the close proximity of the pleura.
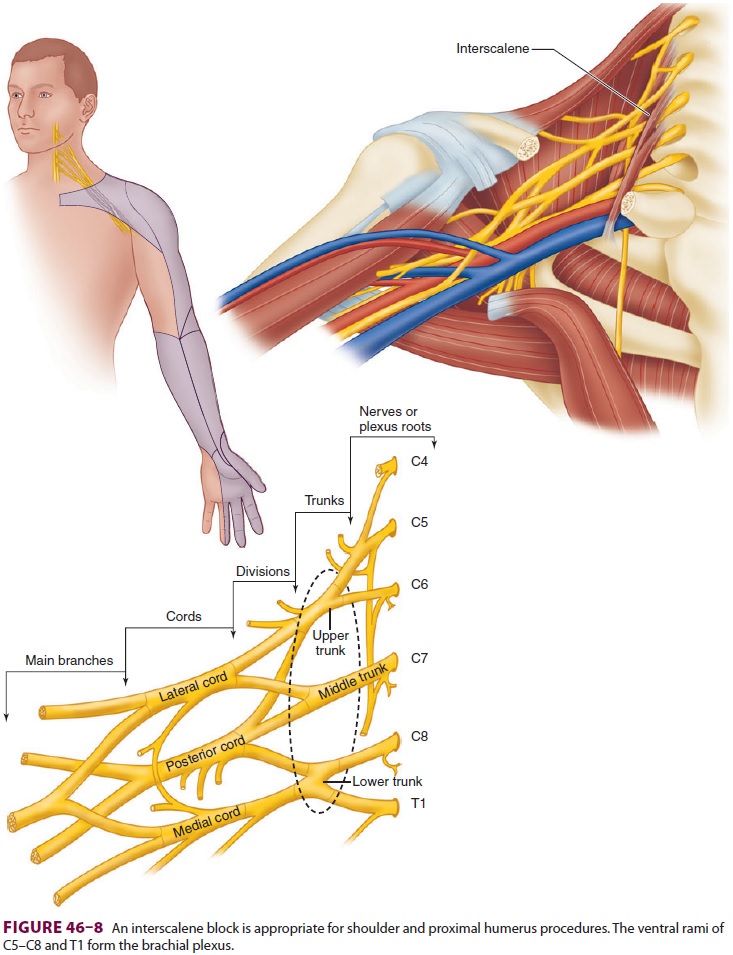
The brachial plexus passes between the anterior
and middle scalene muscles at the level of the cricoid cartilage, or C6 ( Figure
46–9). Palpation of the inter-scalene groove is
usually accomplished with the patient supine and the head rotated 30° or less
to the contralateral side. The external jugular vein often crosses the
interscalene groove at the level of the cricoid cartilage. The interscalene
groove should not be confused with the groove between the sternoclei-domastoid
and the anterior scalene muscle, which lies further anterior. Having the
patient lift and turn the head against resistance often helps delineate the
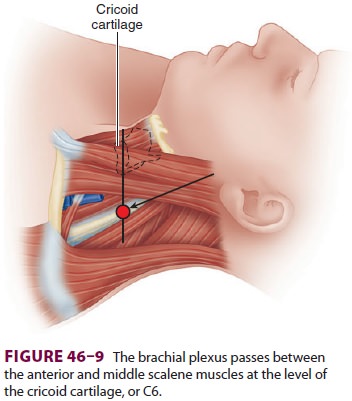
anatomy. If surgical anesthesia is desired
for the entire shoulder, the intercostobrachial nerve must usually be targeted
separately with a field block since it originates from T2 and is not affected
with an interscalene block. Interscalene perineural infusions provide potent
analgesia following shoulder surgery.
A. Nerve Stimulation
relatively short (5-cm) insulated needle is
usu-ally employed. The interscalene groove is palpated using the nondominant
hand, pressing firmly to stabilize the skin against the underlying structures (Figure
46–10). After the skin is anesthetized, the block
needle is inserted at a slightly medial and cau-dad angle and advanced to
optimally elicit a motor response of the deltoid or biceps muscles (suggesting
stimulation of the superior trunk). A motor response of the diaphragm indicates
that the needle is placed in too anterior a direction; a motor response of the
trapezius or serratus anterior muscles indicates that the needle is placed in
too posterior a direction. If bone (transverse process) is contacted, the
needle should be redirected more anteriorly. Aspiration of arterial blood
should raise concern for vertebral or carotid artery puncture; the needle
should be
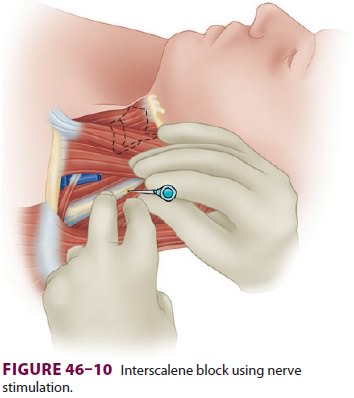
withdrawn, pressure held for 3–5 min, and land-marks reassessed.
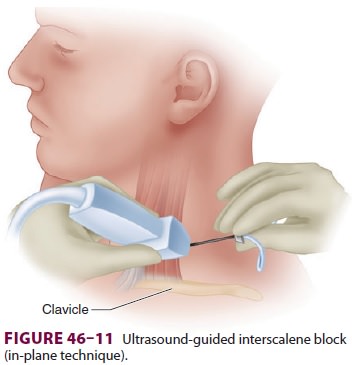
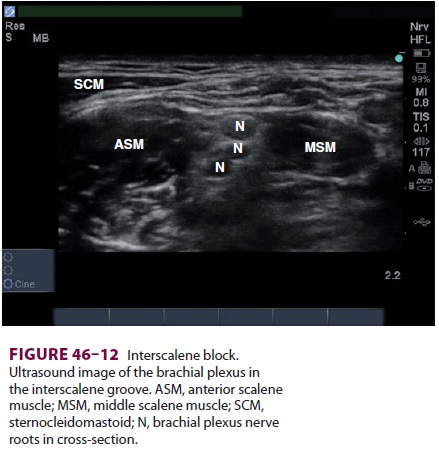
B. Ultrasound
A needle in-plane or out-of-plane technique
may be used, and an insulated needle attached to a nerve stimulator can be used
to confirm the accuracy of the targeted structure. For both techniques, after
identification of the sternocleidomastoid muscle and interscalene groove at the
approximate level of C6, a high-frequency linear transducer is placed
perpendicular to the course of the interscalene mus-cles (short axis; Figure
46–11). The brachial plexus and anterior and
middle scalene muscles should be visualized in cross-section (Figure
46–12). The brachial plexus at this level appears
as three to five hypoechoic circles. The carotid artery and internal jugular
vein may be seen lying anterior to the ante-rior scalene muscle; the
sternocleidomastoid is vis-ible superficially as it tapers to form its lateral
edge.
For an out-of-plane technique, the block nee-dle is inserted just
cephalad to the transducer and advanced in a caudal direction toward the
visual-ized plexus. After careful aspiration for nonappear-ance of blood, local
anesthetic (hypoechoic) spread
should occur adjacent to (sometimes surrounding) the plexus.
For an in-plane technique, the needle is
inserted just posterior to the ultrasound transducer in a direc-tion exactly
parallel to the ultrasound beam. A lon-ger block needle (8 cm) is usually
necessary. It may be helpful to have the patient turn slightly laterally with
the affected side up to facilitate manipulation of the needle. The needle is
advanced through the middle scalene muscle until it has passed through the
fascia anteriorly into the interscalene groove. The needle tip and shaft should
be visualized during the entire block performance. Depending on visu-alized
spread relative to the target nerve(s), a lower volume (10 mL) may be employed
for postoperative analgesia, whereas a larger volume (20–30 mL) is commonly
used for surgical anesthesia.
Related Topics