Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Peripheral Nerve Blocks
Upper Extremity Peripheral Nerve Blocks: Blocks of the Terminal Nerves
Blocks of the Terminal Nerves
Often it is necessary to anesthetize a single ter-minal nerve, either
for minor surgical procedures with a limited field or as a supplement to an
incomplete brachial plexus block. Terminal nerves may be anesthetized anywhere
along their course, but the elbow and the wrist are the two most favored sites.
A. Median Nerve Block
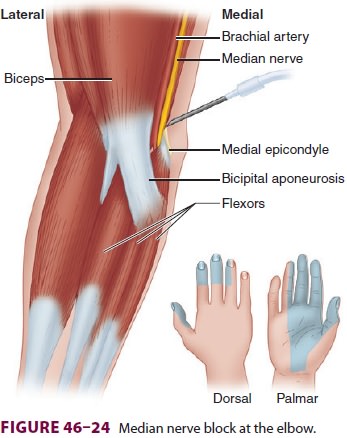
The median nerve is derived from the lateral and medial cords of the
brachial plexus. It enters the arm and runs just medial to the brachial artery (Figure 46-23).
flexors and follows the interosseous membrane to the wrist. At the level
of the proximal wrist flexion crease, it lies directly behind the palmaris longus
tendon in the carpal tunnel.
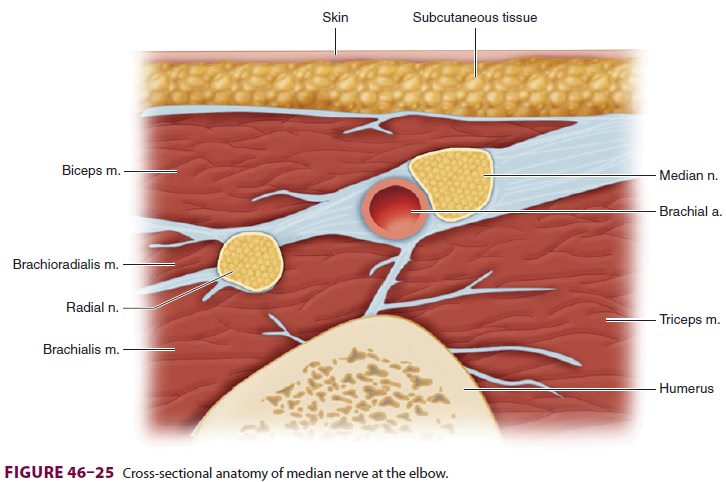
To block the median nerve at the elbow, the brachial artery is
identified in the antecubital crease just medial to the biceps insertion. A
short 22-gauge insulated needle is inserted just medial to the artery and
directed toward the medial epi-condyle until wrist flexion or thumb opposition
is elicited (Figure 46–24); 3–5 mL
of local anesthetic is then injected. If ultrasound is used, the median nerve
may be identified in cross-section just medial to the brachial artery and local
anesthetic injected to surround it (Figure 46–25).
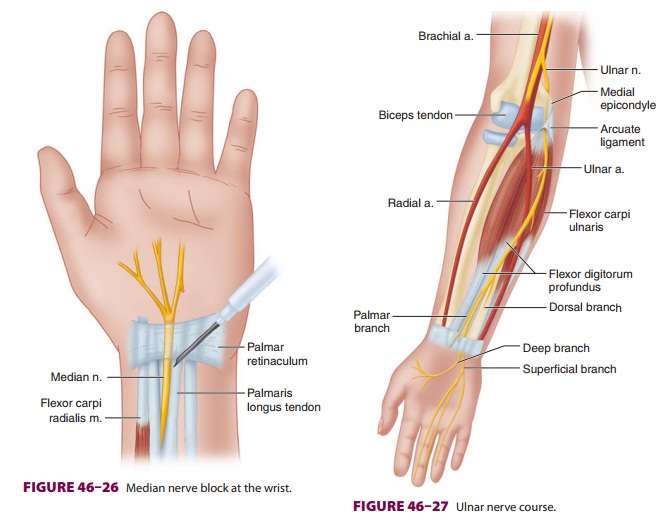
To block the median nerve at the wrist, the palmaris longus tendon is
first identified by ask-ing the patient to flex the wrist against resistance.
short 22-gauge needle is inserted just medial and deep to the palmaris
longus tendon, and 3–5 Ml
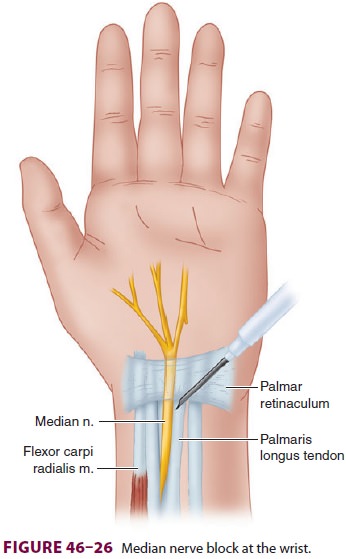
of local anesthetic is injected (Figure 46–26). With ultrasound, the median
nerve may be identified at the level of the mid-forearm between the muscle
bellies of the flexor digitorum profundus, flexor digitorum superficialis, and
flexor pollicis longus (transducer faces perpendicular to the trajectory of the
nerves).
B. Ulnar Nerve Block
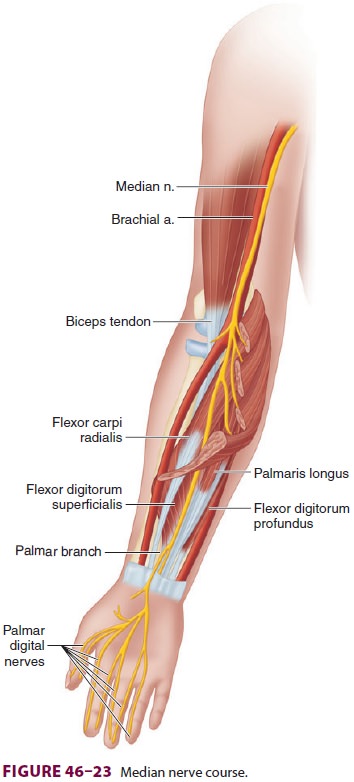
The ulnar nerve is the continuation of the
medial cord of the brachial plexus and maintains a position medial to the
axillary and brachial arteries in the upper arm (Figure 46–27). At the distal third of the humerus, the nerve moves more medially and
passes under the arcuate ligament of the medial epicondyle. The nerve is
frequently palpable just proximal to the medial epicondyle. In the mid-forearm,
the nerve
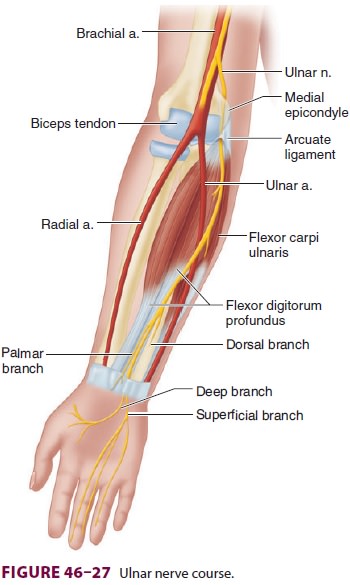
lies between the flexor digitorum profundus and the flexor carpi
ulnaris. At the wrist, it is lateral to the flexor carpi ulnaris tendon and
medial to the ulnar artery.
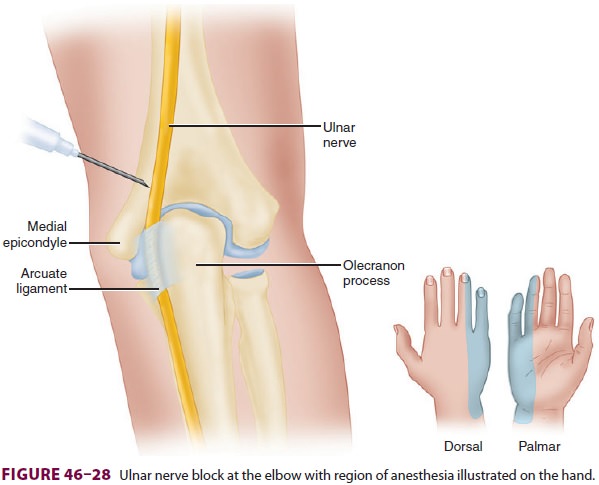
To block the ulnar nerve at the level of the
elbow, an insulated 22-gauge needle is inserted approximately one fingerbreadth
proximal to the arcuate ligament (Figure 46–28), and advanced until fourth/fifth digit flexion or thumb adduction is
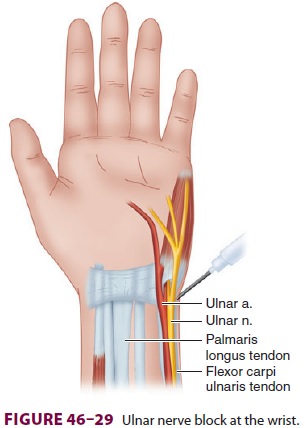
elicited; 3–5 mL of local anesthetic is then injected. To block the ulnar nerve
at the wrist, the ulnar artery pulse is palpated just lateral to the flexor
carpi ulna-ris tendon. The needle is inserted just medial to the artery (Figure
46–29) and 3–5 mL of local anesthetic is injected.
If ultrasound is used, the ulnar nerve may be identified just medial to the
ulnar artery.
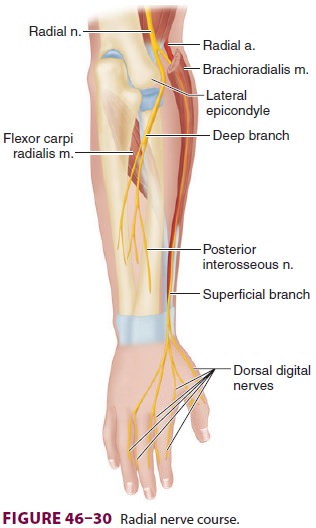
C. Radial Nerve Block
The radial nerve—the terminal branch of the
pos-terior cord of the brachial plexus—courses poste-rior to the humerus,
innervating the triceps muscle, and enters the spiral groove of the humerus
before it moves laterally at the elbow (Figure 46–30). Ter-minal sensory branches include the lateral cutane-ous nerve of
the arm and the posterior cutaneous nerve of the forearm. After exiting the
spiral groove as it approaches the lateral epicondyle, the radial nerve
separates into superficial and deep branches. The deep branch remains close to
the periosteum and innervates the postaxial extensor group of the forearm. The
superficial branch becomes superficial and follows the radial artery to
innervate the radial aspects of the dorsal wrist and the dorsal aspect of the
lateral three digits and half of the fourth.
To block the radial nerve at the elbow, the
biceps tendon is identified in the antecubital fossa. A short 22-gauge
insulated needle is inserted just lateral to the tendon and directed toward the
lateral
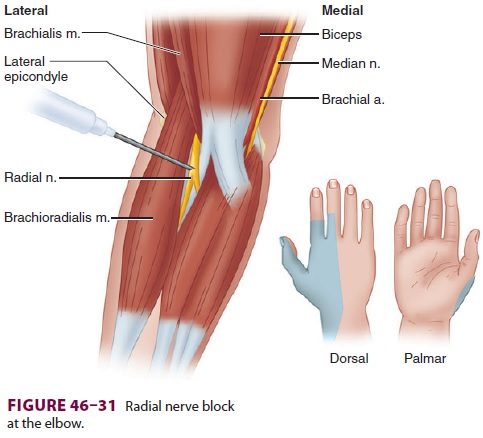
epicondyle (Figure 46–31) until wrist or finger
extension is elicited; 5 mL of local anesthetic is then injected. With
ultrasound, the radial nerve can be identified in cross-section just proximal
to the ante-cubital fossa between the biceps and brachioradialis muscles.
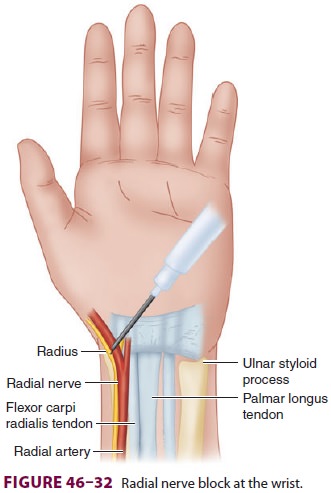
At the wrist, the superficial branch of the
radial nerve lies just lateral to the radial artery, which can be easily palpated
lateral to the flexor carpi radia-lis tendon (Figure 46–32). Using a short 22-gauge needle, 3–5 mL local anesthetic is injected
lateral to the artery. Ultrasound may be used at the level of the wrist or
mid-forearm to identify the radial nerve just lateral to the radial artery.
D. Musculocutaneous Nerve Block
A musculocutaneous nerve block is essential to complete the anesthesia
for the forearm and wrist and is commonly included when performing the axillary
block. The musculocutaneous nerve is the terminal branch of the lateral cord
and the most proximal of the major nerves to emerge from the brachial plexus (Figure
46–33). This nerve inner-vates the biceps and brachialis muscles and distally
terminates as the lateral antebrachial cutaneous nerve, supplying sensory input
to the lateral aspect of the forearm and wrist.
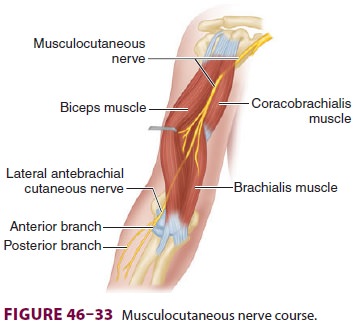
To target the musculocutaneous nerve follow-ing an axillary block, the
needle is redirected supe-rior and proximal to the artery (see Figure 46–21),
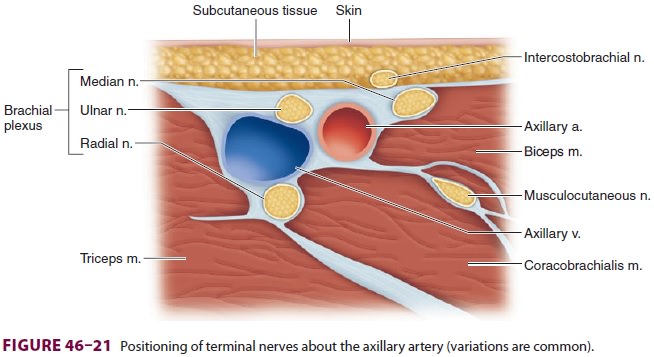
the coracobrachialis muscle is pierced, and
5–10 mL of local anesthetic is injected, with or without elici-tation of elbow
flexion. (Simple infiltration may be used, although the success rate using this
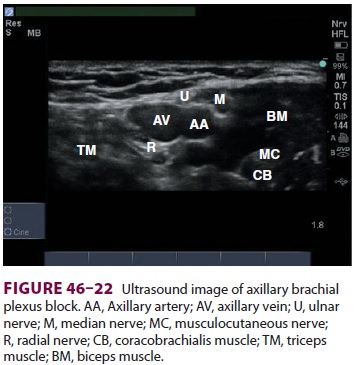
technique is questionable.) Ultrasound may be used to con-firm the location of
the musculocutaneous nerve in the coracobrachialis muscle or between this
muscle and the biceps (see Figure 46–22). Alternatively, the block can be
performed at the elbow as the nerve courses superficially at the
interepicondylar line. The insertion of the biceps tendon is identified,
andshort 22-guage needle is inserted 1–2 cm later-ally; 5–10 mL of local anesthetic
is then injected as field block.
E. Digital Nerve Blocks
Digital nerve blocks are used for minor
operations on the fingers and to supplement incomplete brachial plexus and
terminal nerve blocks. Sensory innerva-tion of each finger is provided by four
small digital nerves that enter each digit at its base in each of the four
corners (Figure 46–34). A small-gauge needle
is inserted at the medial and lateral aspects of the base of the selected
digit, and 2–3 mL of local anesthetic

is inserted without epinephrine. Addition of a vaso-constrictor (epinephrine)
has been claimed to seri-ously compromise blood flow to the digit; however,
there are no case reports involving lidocaine or other modern local anesthetics
to confirm this claim.
F. Intercostobrachial Nerve Block
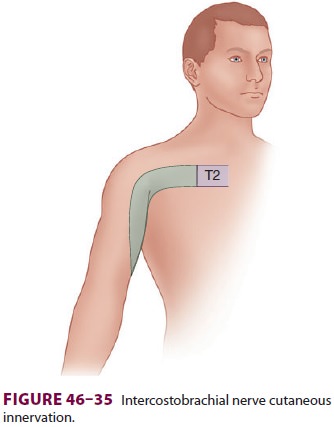
The intercostobrachial nerve originates in
the upper thorax (T2) and becomes superficial on the medial upper arm. It
supplies cutaneous innervation to the medial aspect of the proximal arm and is not anes-thetized with a brachial plexus
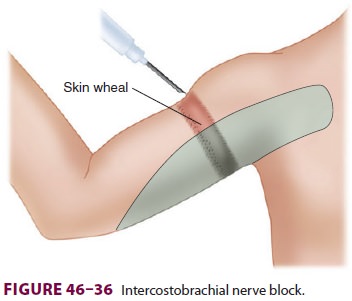
block ( Figure 46–35). The patient should be
supine with the arm abducted and externally rotated. Starting at the deltoid
promi-nence and proceeding inferiorly, a field block is performed in a linear
fashion using 5 mL of local anesthetic, extending to the most inferior aspect
of the medial arm ( Figure 46–36).
Related Topics