Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Peripheral Nerve Blocks
Peripheral Nerve Blocks: Block Techniques
BLOCK TECHNIQUES
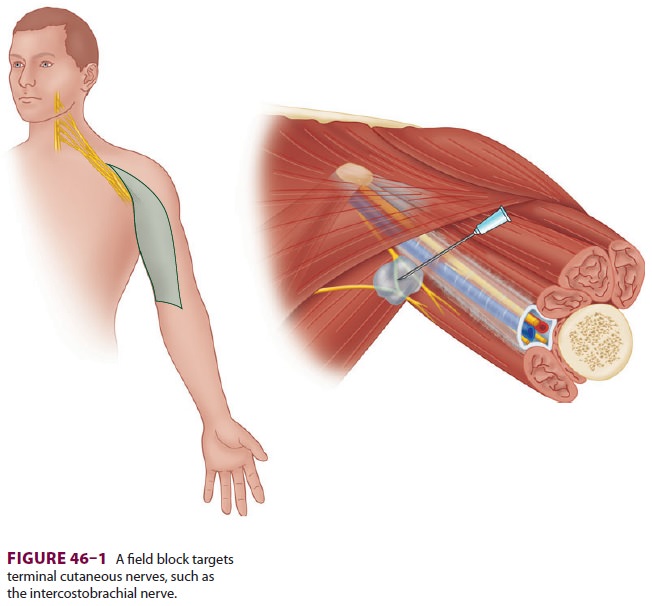
Field Block Technique
A field
block is a local anesthetic injection that tar-gets terminal cutaneous
nerves (Figure 46–1). Field blocks are used
commonly by surgeons to minimize incisional pain and may be used as a
supplementary technique or as a sole anesthetic for minor, super-ficial
procedures. Anesthesiologists often use field blocks to anesthetize the
superficial cervical plexus for procedures involving the neck or shoulder; the
intercostobrachial nerve for surgery involving the medial upper extremity
proximal to the elbow (in combination with a brachial plexus nerve block); and
the saphenous nerve for surgery involving the medial leg or ankle joint (in
combination with a sci-atic nerve block). Field blocks may be undesirable in
cases where they obscure the operative anatomy, or where local tissue acidosis
from infection prevents effective local anesthetic functioning.
Paresthesia Technique
Formerly the mainstay of regional anesthesia, this technique is now
rarely used for nerve localiza-tion. Using known anatomic relationships and
sur-face landmarks as a guide, a block needle is placed in proximity to the
target nerve or plexus. When a needle makes direct contact with a sensory
nerve, a paresthesia (abnormal sensation) is elicited in its area of sensory
distribution.
Nerve Stimulation Technique
For this technique, an insulated needle
concen-trates electrical current at the needle tip, while a wire attached to
the needle hub connects to a nerve stimulator—a battery-powered machine that
emits a small amount (0–5 mA) of electric current at a set interval (usually 1
or 2 Hz). A grounding electrode is attached to the patient to complete the
circuit (Figure 46–2). When the insulated
needle is placed in
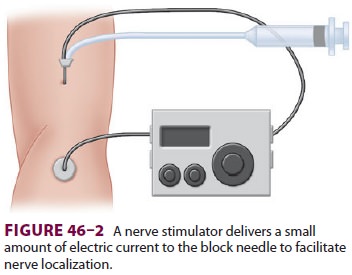
proximity to a motor nerve, muscle contractions
are induced, and local anesthetic is injected. Although it is common to
redirect the block needle until muscle contractions occur at a current less
than 0.5 mA, there is scant evidence to support this specific cur-rent in all
cases. Similarly, although some have sug-gested that muscle contraction with
current less than 0.2 mA implies intraneural needle placement, there is little
evidence to support this specific cutoff. Nonetheless, most practitioners
inject local anes-thetic when current between 0.2 and 0.5 mA results in a
muscle response. For most blocks using this technique, 30–40 mL of anesthetic
is usually injected with gentle aspiration between divided doses.
Ultrasound Technique
Ultrasound for peripheral nerve localization
is becoming increasingly popular; it may be used alone or combined with other
modalities such as nerve stimulation. Ultrasound uses high-frequency (1–20 MHz)
sound waves emitted from piezoelectric crys-tals that travel at different rates
through tissues of dif-ferent densities, returning a signal to the transducer.
Depending on the amplitude of signal received, the crystals deform to create an
electronic voltage that is converted into a two-dimensional grayscale image.
The degree of efficiency with which sound passes through a substance determines
its echogenicity. Structures and substances through which sound passes easily
are described as hypoechoic and
appear dark or black on the ultrasound screen. In contrast, structures
reflecting more sound waves appear brighter—or white—on the ultrasound screen,
and are termed hyperechoic.
The optimal transducer varies depending upon the depth of the target
nerve and approach angle of the needle relative to the transducer (Figure
46–3). High-frequency transducers provide a high-res-olution picture with a
relatively clear image but
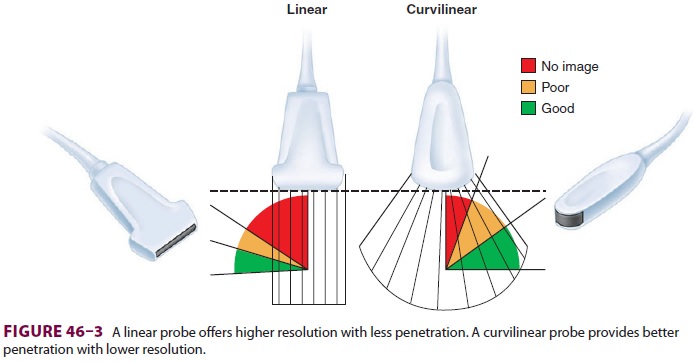
offer poor tissue penetration and are therefore used predominantly for
more superficial nerves. Low-frequency transducers provide an image of poorer
quality but have better tissue penetration and are therefore used for deeper
structures. Transducers with a linear array offer an undistorted image and are
therefore often the first choice among practitio-ners. However, for deeper target
nerves that require
more acute angle between the needle and
long-axis of the transducer, a curved array (curvilinear) trans-ducer will
maximize returning ultrasound waves, providing the optimal needle image (Figure
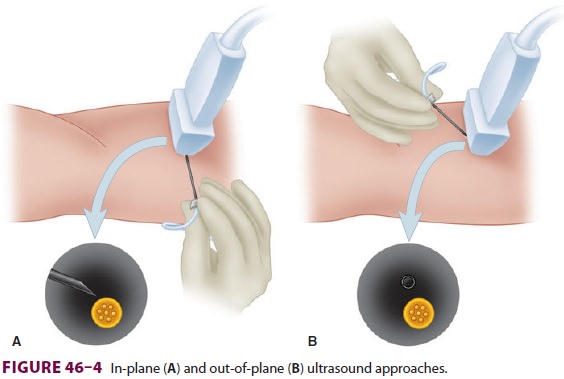
46–3). Nerves are best imaged in cross-section, where they have a
characteristic honeycomb appearance (“short axis”). Needle insertion can pass
either par-allel (“in plane”) or not parallel (“out of plane”) to the plane of
the ultrasound waves (Figure 46–4).
Unlike nerve stimulation alone, ultrasound guid-ance allows for a variable
volume of local anesthetic to be injected, with the final amount determined by
what is observed under direct vision. This technique usually results in a far
lower injected volume of local anesthetic (10–30 mL).
Continuous Peripheral Nerve Blocks
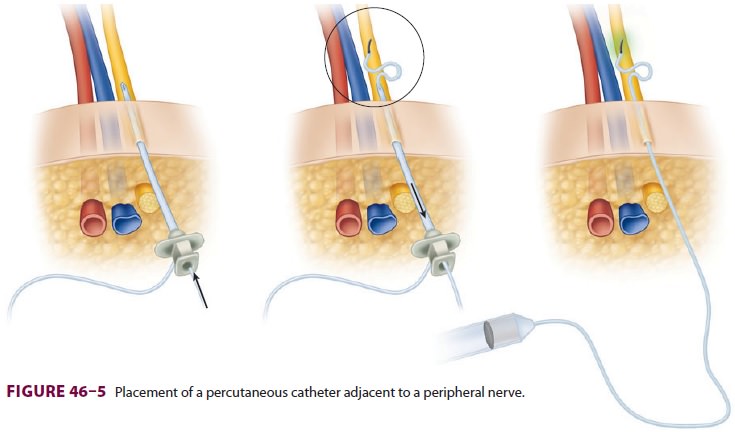
Also termed perineural local
anesthetic infusion, continuous peripheral nerve blocks involve the
placement of a percutaneous catheter adjacent to a peripheral nerve, followed
by local anes-thetic administration to prolong a nerve block (Figure
46–5). Potential advantages appear to depend on successfully improving
analgesia and include reductions in resting and dynamic pain, sup-plemental
analgesic requirements, opioid-related side effects, and sleep disturbances. In
some cases patient satisfaction, ambulation, and functioning may be improved;
an accelerated resumption of passive joint range-of-motion realized; and
reduced time until discharge-readiness as well as actual dis-charge from the
hospital or rehabilitation center achieved.
Th ere are many types of catheters, including nonstimulating and
stimulating, flexible and more rigid, through-the-needle and over-the-needle.
Currently, there is little evidence that a single design results in superior
effects. Local anesthetic is the primary medication infused, as adjuvants do
not add benefits to perineural infusions (unlike single-injection peripheral
nerve blocks). Long-acting local anesthetics (eg, ropivacaine) are more
commonly used as they provide a more favorable sensory-to-motor block ratio
(optimizing analgesia while minimizing motor block). In an attempt to further
minimize any induced motor block, dilute
local anesthetic (0.1–0.2%) is often infused;
how-ever, recent evidence suggests that it is the total dose, and not
concentration, that determines the major-ity of block effects. Unlike single-injection peripheral nerve
blocks, no adjuvant added to a perineural local anesthetic infusion has been demonstrated to be of benefit. The local
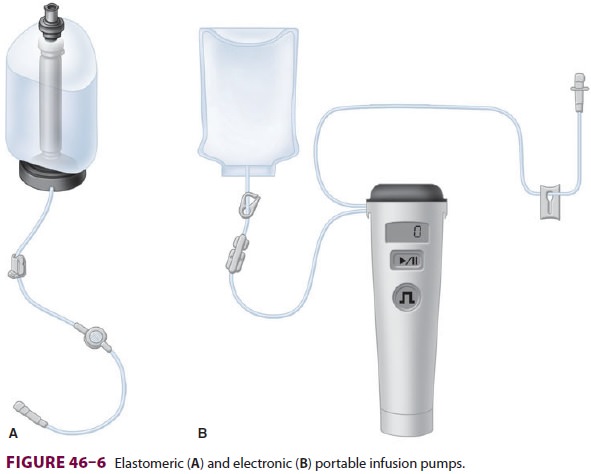
anesthetic may be administered exclusively as repeated bolus doses or a basal
infu-sion, or as a combination of the two methods. Using a small, portable
infusion pump (Figure 46–6), con-tinuous
peripheral nerve blocks may be provided on an ambulatory basis.
As with all medical procedures, there are
potential risks associated with continuous periph-eral nerve blocks. Therefore,
these infusions are usually reserved for patients having procedures expected to
result in postoperative pain that is dif-ficult to control with oral analgesics
and will not resolve in less time than the duration of a single-injection
peripheral nerve block. Serious compli-cations, which are relatively rare,
include systemic local anesthetic toxicity, catheter retention, nerve injury,
infection, and retroperitoneal hematoma formation. In addition, a perineural
infusion affect-ing the femoral nerve increases the risk of fall-ing, although
to what degree and by what specific mechanism (eg, sensory, motor, or
proprioception deficits) remain unknown.
Related Topics