Chapter: Clinical Anesthesiology: Regional Anesthesia & Pain Management: Peripheral Nerve Blocks
Peripheral Nerve Blocks of the Trunk: Paravertebral Block
Paravertebral Block
Paravertebral blocks provide surgical anesthesia or postoperative
analgesia for procedures involving the thoracic or abdominal wall, mastectomy,
ingui-nal or abdominal hernia repair, and more invasive unilateral procedures
such as open nephrectomy. Paravertebral blocks usually require individual
injections delivered at the various vertebral levels that correspond to the
area of body wall to be anes-thetized. For example, a simple mastectomy would
require blocks at levels T3–6; for axillary node dis-section, additional
injections should be made from C7 through T2. For inguinal hernia repair,
blocks should be performed at T10 through L2. Ventral hernias require bilateral
injections corresponding to the level of the surgical site. The major
com-plication of thoracic injections is pneumothorax, whereas retroperitoneal
structures may be at risk with lumbar-level injections. Hypotension sec-ondary
to sympathectomy can be observed with multilevel thoracic blocks. Unlike the
intercostal approach, long-acting local anesthetic will have a nearly 24-hour
duration, and perineural catheterinsertion is a viable option (although local
anes-thetic spread from a single catheter to multiple lev-els is variable).
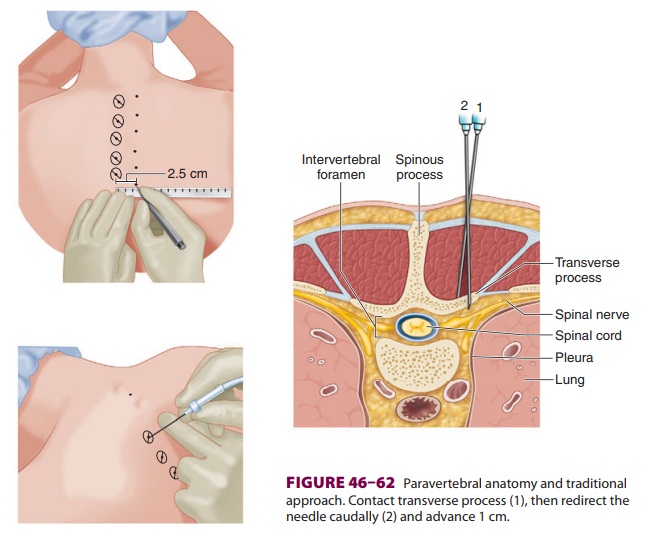
Each spinal nerve emerges from the
interverte-bral foramina and divides into two rami: a larger anterior ramus,
which innervates the muscles and skin over the anterolateral body wall and
limbs, and a smaller posterior ramus, which reflects posteriorly and innervates
the skin and muscles of the backand neck (Figure 46–62). The thoracic
para-vertebral space is defined posteriorly by thesuperior costotransverse
ligament, anterolaterally by the parietal pleura, medially by the vertebrae and
the intervertebral foramina, and inferiorly and superi-orly
by the heads of the ribs.
With the patient seated and vertebral column
flexed, each spinous process is palpated, counting from the prominent C7 for
thoracic blocks, and the iliac crests as a reference for lumbar levels. From
the midpoint of the superior aspect of each spinous process, a point 2.5 cm
laterally is measured and marked. In the thorax, the target nerve is located
lat-eral to the spinous process above
it, due to the steep
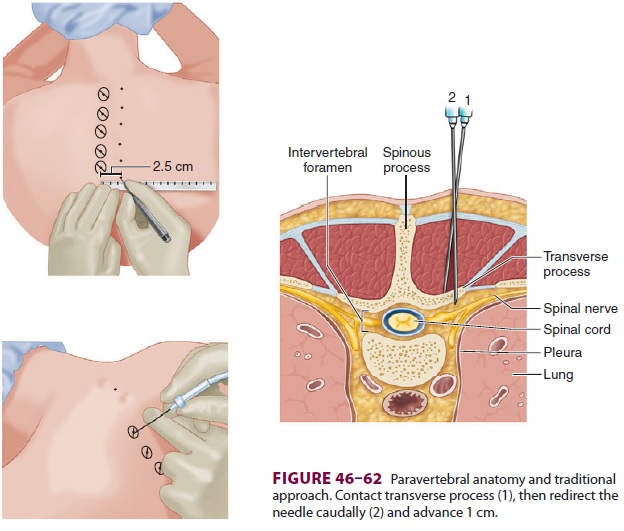
angulation of thoracic spinous processes (eg, the T4 nerve root is
located lateral to the spinous process of T3).
A. Traditional Technique
A pediatric Tuohy needle (20 gauge) is
inserted at each point and advanced perpendicular to the skin (Figure 46–62).
Upon contact with the transverse process, the needle is withdrawn slightly and
redi-rected caudally an additional 1 cm (0.5 cm for lum-bar placement). A “pop”
or loss of resistance may be felt as the needle passes through the
costotransverse ligament. Some practitioners use a loss-of-resistance syringe
to guide placement; others prefer use of a nerve stimulator with chest wall
motion for the end point. Inject 5 mL of local anesthetic at each level. The difficulty
with this technique is that the depth of the transverse process is simply
estimated; thus the risk of pneumothorax is relatively high. Using ultrasound
to gauge transverse process depth prior to needle insertion theoretically
decreases the risk of pneumothorax.
B. Ultrasound
An ultrasound transducer with a curvilinear array is used, with the beam oriented in a parasagittal or transverse plane. The transverse process, head of the rib, costotransverse ligament, and pleura are iden-tified. The paravertebral space may be approached from a caudal-to-cephalad direction (parasagittal) or a lateral-to-medial direction (transverse). It is helpful to visualize the needle in-plane as it passes through the costotransverse ligament and observe a downward displacement of the pleura as local anes-thetic is injected. At each level 5 mL of local anes-thetic is injected.
Related Topics