Chapter: Biochemical Pharmacology : Drugs that act on sodium and potassium channels
Overview of the autonomic nervous system
Overview of the autonomic
nervous system
It was stated at the
beginning that the peripheral autonomic system has a prominent place as a site
of drug action. We will now look at the organization of this system, and at the
distribution of transmitter receptors within it. This will enable us to
understand the effects of drugs acting upon this system and rationales behind
their usage.
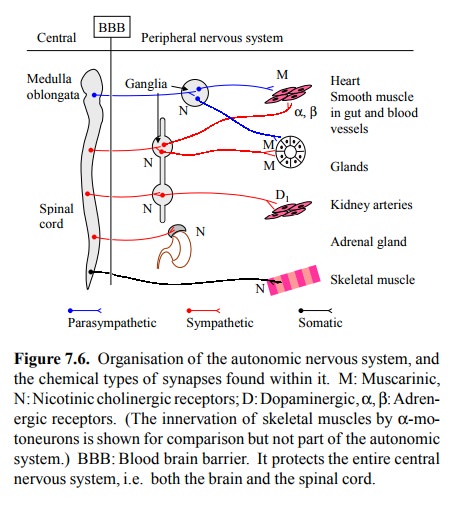
The autonomic nervous system
consists of two function-ally distinct parts that frequently exert antagonistic
effects on their target organs. These are referred to as the sympa-thetic and
the parasympathetic system, respectively. Figure 7.6 depicts some essential
features. The parasympathet-ic system, for the most part, emerges from the
central ner-vous system at the level of the medulla
oblongata, which is the lowermost part of the brain. These neurons reach
some nerve centers in the periphery, which are named gan-glia (singular: ganglion),
where they trigger activity in sec-ondary neurons that in turn reach out to the
target organs. The sympathetic system mostly emerges at the thoracic portion of
the spinal cord. It too has relay neurons in pe-ripheral ganglia (which are
connected with each other in the so-called `sympathetic chains', located on
either side of the spine). The parasympathetic and sympathetic ganglia are
outside the central nervous system, and therefore readi-ly accessible to drugs
that do not cross the blood brain bar-rier.
The target tissues that are
controlled by the secondary neurons (the ones originating in the ganglia)
include:
• Secretory cells in various glands, both
exocrine and endocrine;
• Heart conduction system and muscle cells;
• Smooth muscle cells in in the intestine, other
hollow organs (bronchi, urinary tract, sexual organs, etc.) and in the blood
vessels.
Figure 7.6 also shows the major types of
neurotransmitter receptors found within the autonomic nervous system:
The nicotinic acetylcholine
receptor occurs in both the sympathetic and the parasympathetic ganglia. The
re-ceptors found in the neuromuscular synapse are of the nicotinic type as
well. However, the subtype is different, and therefore selective drug action is
possible.
• Muscarinic acetylcholine receptors occur in the
tar-get tissues. They are mostly found in parasympathetic synapses, but they
also occur in the sympathetically in-nervated sweat glands.
• Adrenergic receptors are always related to
sympathet-ic activity, either within synapses (as shown here), or diffusely
distributed and by responding to circulat-ing epinephrine.
• Dopamine D1 receptors are less
widespread than adren-ergic receptors. One prominent occurrence is in the
kid-ney arteries. Accordingly, dopamine and related ago-nists are being used in
intensive care treatment of acute kidney failure to improve kidney perfusion.
Very commonly, a target
tissue will be stimulated by the sympathetic system and inhibited by the
parasympathet-ic system, or vice versa. Examples are found in table 7.1. Among
the parasympathetic responses listed there, we find stimulation of smooth
muscle in the bronchi, and relax-ation of smooth muscle in the arterioles; both
are mediat-ed by muscarinic acetylcholine receptors (cf. Figure 7.6). Here, we
have an example of diverse effector mechanisms triggered from similar
receptors. Similarly, the adrener-gic receptors can operate different
intracellular switches as needed. These different effector mechanisms are
covered in some more detail in the chapter on G protein-coupled re-ceptors.
nicotinic type as well. However, the subtype is different, and therefore
selective drug action is possible.
• Muscarinic acetylcholine receptors occur in the
tar-get tissues. They are mostly found in parasympathetic synapses, but they
also occur in the sympathetically in-nervated sweat glands.
• Adrenergic receptors are always related to
sympathet-ic activity, either within synapses (as shown here), or diffusely
distributed and by responding to circulat-ing epinephrine.
• Dopamine D1 receptors are less
widespread than adren-ergic receptors. One prominent occurrence is in the
kid-ney arteries. Accordingly, dopamine and related ago-nists are being used in
intensive care treatment of acute kidney failure to improve kidney perfusion.
Very commonly,
a target tissue will be stimulated by the sympathetic system and inhibited by
the parasympathet-ic system, or vice versa. Examples are found in table 7.1.
Among the parasympathetic responses listed there, we find stimulation of smooth
muscle in the bronchi, and relax-ation of smooth muscle in the arterioles; both
are mediat-ed by muscarinic acetylcholine receptors (cf. Figure 7.6). Here, we
have an example of diverse effector mechanisms triggered from similar
receptors. Similarly, the adrener-gic receptors can operate different
intracellular switches as needed. These different effector mechanisms are
covered in some more detail in the chapter on G protein-coupled re-ceptors.

A `take-home' message from
table 7.1 is that, by and large, muscarinic receptors mediate the
parasympathetic effects, whereas the sympathetic ones are mediated by
adrenergic receptors.
From the effects of the
autonomic nervous system on the various target organs (table 7.1), we can
easily understand several applications of drugs that cause synaptic
stimula-tion or inhibition:
• In patients having undergone abdominal surgery,
quite frequently the activity of the intestine is sluggish. Drugs that
stimulate muscarinic receptors will help to cor-rect this.
• As we have seen, drugs that block α-adrenergic re-ceptors (e.g., phenoxybenzamine) will help to lower
the resistance in arterioles and therefore reduce blood pressure.
• Blockers of β1-adrenoceptors help to reduce the work-load of the heart, but they
sometimes slow down the generation or propagation of excitation too much,
re-sulting in slow and occasionally irregular heartbeat.
Drugs that stimulate β2-adrenoceptors
will help to di-late the bronchi (by reducing the smooth muscle tone there)
will be useful in asthma, which basically con-sists in impeded air flow due to
a spastic narrowing of the bronchi.
• If the effect of β2 agonists in asthma proves insufficient, one additional therapeutic
option is to add a drug that will inhibit the cholinergic (parasympathetic)
stimulation of the bronchial smooth muscle, such as ipratropi-um bromide10.
A peculiar element within the
autonomic nervous system is the medulla (inner part) of the adrenal gland. This
is the site of production for epinephrine and norepinephrine that are released
into the circulation. It is directly controlled by cholinergic neurons emerging
from the spinal cord, so it assumes the place of a sympathetic ganglion. In
fact, the cells in the adrenal medulla are of neural origin – they are nerve
cells turned gland cells. In contrast, the cortex (outer part) of the adrenal
gland) is a `proper' gland tissue not of neural but mesodermal origin. The
endocrine (hormonal) and the neural system are not as cleanly separated as our
neat abstractions suggest.11
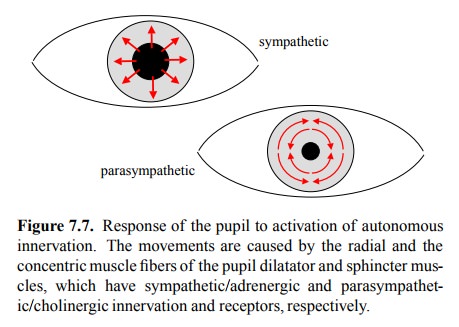
Table 7.1 also lists the
effects of sympathetic and parasym-pathetic stimuli on the pupil of the eye
pupil (this had been omitted from Figure 7.6, which is incomplete in many
ways). In the case of the pupil, the antagonism between sympathetic and
parasympathetic system is due not to an-tagonistic innervation of the same
target cells but of two antagonistic muscles, the dilatator and the sphincter
mus-cles of the iris, respectively (Figure 7.7). While the auto-nomic control
of the iris is not overwhelmingly important in applied pharmacotherapy, it is a
very useful diagnostic marker. E.g., in
poisoning with drugs that induce or amplify cholinergic action we will see a
pronounced narrowing of the pupil. This is called miosis' in doctors' speak;
widening (observed e.g. with cocaine) is `mydriasis'. One of the glorious
things about medicine is the profusion of cryptic names for simple things.
Related Topics