Chapter: Medical Surgical Nursing: Management of Patients With Intestinal and Rectal Disorders
Ulcerative Colitis - Inflammatory Bowel Disease
ULCERATIVE
COLITIS
Ulcerative
colitis is a recurrent ulcerative and inflammatory dis-ease of the mucosal and
submucosal layers of the colon and rec-tum. The incidence of ulcerative colitis
is highest in Caucasians and people of Jewish heritage (Yamada et al., 1999).
The peak in-cidence is between 30 and 50 years of age. It is a serious disease,
accompanied by systemic complications and a high mortality rate. Eventually,
10% to 15% of the patients develop carcinoma of the colon.
Pathophysiology
Ulcerative
colitis affects the superficial mucosa of the colon and is characterized by
multiple ulcerations, diffuse inflammations, and desquamation or shedding of
the colonic epithelium. Bleed-ing occurs as a result of the ulcerations. The
mucosa becomes edematous and inflamed. The lesions are contiguous, occurring
one after the other. Abscesses form, and infiltrate is seen in the mucosa and
submucosa with clumps of neutrophils in the crypt lumens (ie, crypt abscesses).
The disease process usually begins in the rectum and spreads proximally to
involve the entire colon. Eventually, the bowel narrows, shortens, and thickens
because of muscular hypertrophy and fat deposits.
Clinical Manifestations
The
clinical course is usually one of exacerbations and remissions. The predominant
symptoms of ulcerative colitis are diarrhea, lower left quadrant abdominal
pain, intermittent tenesmus, and rectal bleeding. The bleeding may be mild or
severe, and pallor results. The patient may have anorexia, weight loss, fever,
vomit-ing, and dehydration, as well as cramping, the feeling of an ur-gent need
to defecate, and the passage of 10 to 20 liquid stools each day. The disease is
classified as mild, severe, or fulminant, depending on the severity of the
symptoms. Hypocalcemia and anemia frequently develop. Rebound tenderness may
occur in the right lower quadrant. Extraintestinal symptoms include skin
le-sions (eg, erythema nodosum), eye lesions (eg, uveitis), joint
ab-normalities (eg, arthritis), and liver disease.
Assessment and Diagnostic Findings
The
patient should be assessed for tachycardia, hypotension, tachyp-nea, fever, and
pallor. Other assessments include the level of hy-dration and nutritional
status. The abdomen should be examined for characteristics of bowel sounds,
distention, and tenderness. These findings assist in determining the severity
of the disease.
The
stool is positive for blood, and laboratory test results re-veal a low
hematocrit and hemoglobin concentration in addition to an elevated white blood
cell count, low albumin levels, and an electrolyte imbalance. Abdominal x-ray
studies are useful for de-termining the cause of symptoms. Free air in the
peritoneum and bowel dilation or obstruction should be excluded as a source of
the presenting symptoms. Sigmoidoscopy or colonoscopy and barium enema are
valuable in distinguishing this condition from other diseases of the colon with
similar symptoms. A barium enema may show mucosal irregularities, focal
strictures or fistu-las, shortening of the colon, and dilation of bowel loops.
En-doscopy may reveal friable, inflamed mucosa with exudate and ulcerations.
This procedure assists in defining the extent and severity of the disease. CT
scanning, magnetic resonance imag-ing, and ultrasound can identify abscesses
and perirectal in volvement. Leukocyte scanning is useful when se-vere colitis
prohibits the use of endoscopy to determine the ex-tent of inflammation.
Careful
stool examination for parasites and other microbes is performed to rule out
dysentery caused by common intestinal or-ganisms, especially Entamoeba histolytica and Clostridium difficile.
Complications
Complications
of ulcerative colitis include toxic megacolon, per-foration, and bleeding as a
result of ulceration, vascular engorge-ment, and highly vascular granulation
tissue. In toxic megacolon, the inflammatory process extends into the
muscularis, inhibiting its ability to contract and resulting in colonic
distention. Symp-toms include fever, abdominal pain and distention, vomiting,
and fatigue. Colonic perforation from toxic megacolon is asso-ciated with a
high mortality rate (15% to 50%) (Grendell et al., 1998). If the patient with
toxic megacolon does not respond within 24 to 48 hours to medical management
with nasogastric suction, intravenous fluids with electrolytes,
corticosteroids, and antibiotics, surgery is required. Total colectomy is
indicated. For many patients, surgery becomes necessary to relieve the effects
of the disease and to treat these serious complications; an ileostomy usually
is performed. The surgical procedures involved and the care of patients with
this type of fecal diversion are discussed later.
Patients
with IBD also have a significantly increased risk of os-teoporotic fractures
due to decreased bone mineral density. Corti-costeroid therapy may also
contribute to the diminished bone mass.
Medical Management of Chronic Inflammatory Bowel Disease
Medical
treatment for regional enteritis and ulcerative colitis is aimed at reducing
inflammation, suppressing inappropriate im-mune responses, providing rest for a
diseased bowel so that heal-ing may take place, improving quality of life, and
preventing or minimizing complications.
Most
patients maintain long-term well-being interspersed with short intervals of
illness (Hanauer, 2001). Management depends on the disease location, severity,
and complications.
NUTRITIONAL THERAPY
Oral
fluids and a low-residue, high-protein, high-calorie diet with supplemental
vitamin therapy and iron replacement are prescribed to meet nutritional needs,
reduce inflammation, and control pain and diarrhea. Fluid and electrolyte
imbalances from dehydration caused by diarrhea are corrected by intravenous
therapy as neces-sary if the patient is hospitalized or by oral supplementation
if the patient can be managed at home. Any foods that exacerbate diar-rhea are
avoided. Milk may contribute to diarrhea in those with lactose intolerance.
Cold foods and smoking are avoided because both increase intestinal motility.
Parenteral nutrition may be indicated.
PHARMACOLOGIC THERAPY
Sedatives
and antidiarrheal and antiperistaltic medications are used to minimize
peristalsis to rest the inflamed bowel. They are continued until the patient’s
stools approach normal frequency and consistency.
Aminosalicylate
formulations such as sulfasalazine (Azulfidine) are often effective for mild or
moderate inflammation and are used to prevent or reduce recurrences in
long-term maintenance regi-mens. Newer sulfa-free aminosalicylates (eg,
mesalamine [Asacol, Pentasa]) have been developed and shown effective in
preventing and treating recurrence of inflammation (Wolfe, 2000). Anti-biotics
are used for secondary infections, particularly for purulent complications such
as abscesses, perforation, and peritonitis.
Corticosteroids
are used to treat severe and fulminant disease. These corticosteroids (eg,
prednisone) can be administered orally in outpatient treatment or parenterally
in hospitalized patients. Topical (ie, rectal administration) corticosteroids
are also widely used in the treatment of distal colon disease. When the dosage
of corticosteroids is reduced or stopped, the symptoms of disease may return.
If corticosteroids are continued, adverse sequelae such as hypertension, fluid
retention, cataracts, hirsutism (ie, abnormal hair growth), adrenal
suppression, and loss of bone density may develop.
Immunomodulators
(eg, azathioprene [Imuran], 6-mercap-topurine, methotrexate, cyclosporin) have
been used to alter the immune response (Wolfe, 2000). The exact mechanism of
action of these medications in treating IBD is unknown. They are used for
patients with severe disease who have failed other therapies. These medications
are useful in maintenance regimens to prevent relapses. Newer biologic
therapies are being studied, and it is hoped that they will lead to improvement
in the treatment of pa-tients with chronically active disease (Yamada et al.,
1999).
SURGICAL MANAGEMENT
When
nonsurgical measures fail to relieve the severe symptoms of IBD, surgery may be
recommended. The most common indications for surgery are medically intractable
disease, poor quality of life, or complications from the disease or medical
ther-apy (Wolfe, 2000).
More
than one half of all patients with regional enteritis require surgery at some
point. Recurrence of inflammation and disease after surgery in regional
enteritis is inevitable. The rate of recur-rence after surgery is 20% to 40% in
the first 5 years. Patients younger than 25 years of age have the highest
recurrence rate. Surgery for regional enteritis is indicated for refractory
disease or complications (Wolfe, 2000). The procedure of choice is a total
colectomy and ileostomy.
A
newer surgical procedure developed for patients with severe regional enteritis
is intestinal transplant. This technique is now available to children and to
young and middle-age adults who have lost intestinal function from disease.
Although not a cure, this procedure may eventually provide improvement in
quality of life for some who are terminally ill. The technical and immunologic
problems with this procedure remain formidable, and the costs and mortality
rates remain high (Wolfe, 2000).
Approximately
15% to 20% of patients with ulcerative coli-tis require surgical intervention
(Tierney et al., 2000). Indica-tions for surgery include lack of improvement
and continued deterioration, profuse bleeding, perforation, stricture
formation, and cancer. Surgical excision usually improves quality of
life.Proctocolectomy with ileostomy (ie, complete excision of colon, rectum,
and anus) is recommended when the rectum is severely involved.
One
type of surgical technique that can be helpful is stric-tureplasty, in which
the blocked or narrowed section of the bowel is widened, leaving the bowel
intact. If a lesion can be delineated in regional enteritis or if a
complication has occurred, the lesion is resected, and the remaining portions
of the bowel are anasto-mosed. Surgical removal of up to 50% of the small bowel
usually can be tolerated. Other types of surgical procedures, known as fecal
diversions, are discussed later.
Total Colectomy With Ileostomy.
Anileostomy, the surgical cre-ation of an
opening into the ileum or small intestine (usually by means of an ileal stoma
on the abdominal wall), is commonly per-formed after a total colectomy (ie,
excision of the entire colon). It allows for drainage of fecal matter (ie,
effluent) from the ileum to the outside of the body. The drainage is very mushy
and oc-curs at frequent intervals. Nursing management of the patient with an ileostomy
is discussed in a later section.
Total Colectomy With Continent Ileostomy.
Another procedureinvolves the removal of the entire colon and creation
of the con-tinent ileal reservoir (ie, Kock pouch). This procedure eliminates
the need for an external fecal collection bag. Approximately 30 cm of the
distal ileum is reconstructed to form a reservoir with a nipple valve that is
created by pulling a portion of the terminal ileal loop back into the ileum. GI
effluent can accumulate in the pouch for several hours and then be removed by
means of a catheter inserted through the nipple valve. The major problem with
the Kock pouch is malfunction of the nipple valve, which occurs in about 20% of
the patients (Yamada et al., 1999).
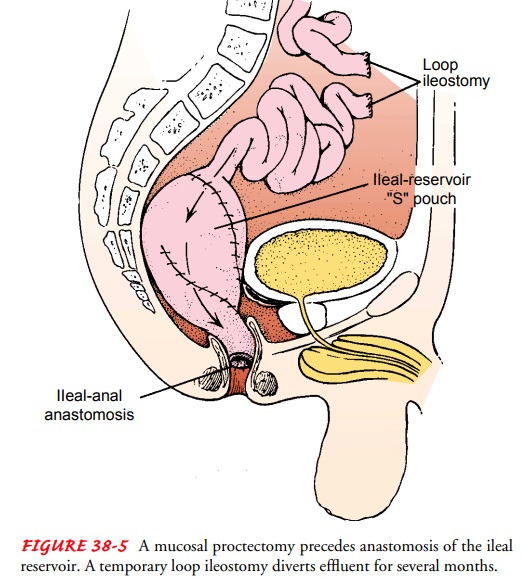
Total Colectomy With Ileoanal Anastomosis.
A total colectomywith ileoanal anastomosis is another surgical procedure
that elim-inates the need for a permanent ileostomy. It establishes an ileal
reservoir, and anal sphincter control of elimination is retained. The procedure
involves connecting a portion of the ileum to the anus (ie, ileoanal
anastomosis) in conjunction with removal of the colon and the rectal mucosa
(ie, total abdominal colectomy and mucosal proctectomy) (Fig. 38-5). A
temporary diverting loop ileostomy is constructed at the time of surgery and
closed about 3 months later.
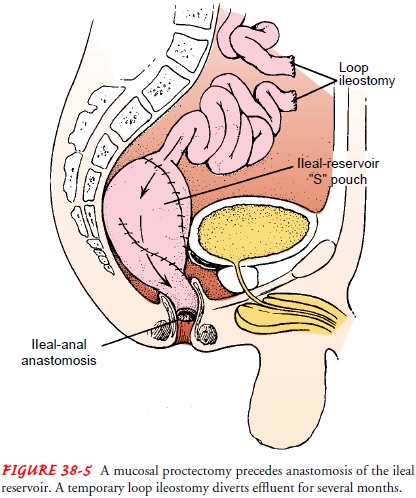
With
ileoanal anastomosis, the diseased colon and rectum are re-moved, voluntary
defecation is maintained, and anal continence is preserved. The ileal reservoir
decreases the number of bowel move-ments by 50%, from approximately 14 to 20
per day to 7 to 10 per day. Nighttime elimination is gradually reduced to one
bowel movement. Complications of ileoanal anastomosis include irritation of the
perianal skin from leakage of fecal contents, stricture forma-tion at the
anastomosis site, and small bowel obstruction.
Nursing Management
Nursing management of patients with IBD may be medical, sur-gical, or both. Patients in the community setting or those recently diagnosed may primarily require education about diet and med-ications and referral to support groups. Hospitalized patients with long-standing or severe disease also require careful monitoring, parenteral nutrition, fluid replacement, and possibly emergent surgery. The surgical procedures may involve a fecal diversion, with attendant needs for physical care, emotional support, and extensive teaching about management of the ostomy.
Related Topics