Chapter: Medical Surgical Nursing: Management of Patients With Intestinal and Rectal Disorders
Nursing Management of the Patient Requiring an Ileostomy
NURSING
MANAGEMENT OF THE PATIENT REQUIRING AN ILEOSTOMY
Some
patients with IBD eventually require permanent fecal di-version with creation
of an ileostomy to manage symptoms and to treat or prevent complications. The
Plan of Nursing Care 38-1 summarizes care for the patient requiring an ostomy.
Providing Preoperative Care
A
period of preparation with intensive replacement of fluid, blood, and protein
is necessary before surgery is performed. Anti-biotics may be prescribed. If
the patient has been taking corti-costeroids, they will be continued during the
surgical phase to prevent steroid-induced adrenal insufficiency. Usually, the
patient is given a low-residue diet, provided in frequent, small feedings. All
other preoperative measures are similar to those for general abdominal surgery.
The abdomen is marked for the proper place-ment of the stoma by the surgeon or
the enterostomal therapist. Care is taken to ensure that the ostomy stoma is
conveniently placed–usually in the right lower quadrant about 2 inches below
the waist, in an area away from previous scars, bony prominence, skin folds, or
fistulas.
The
patient must have a thorough understanding of the surgery to be performed and
what to expect after surgery. Infor-mation about an ileostomy is presented to
the patient by means of written materials, models, and discussion. Preoperative
teach-ing includes management of drainage from the stoma, the nature of
drainage, and the need for nasogastric intubation, parenteral fluids, and
possibly perineal packing.
Providing Postoperative Care
General
abdominal surgery wound care is required. The nurse observes the stoma for
color and size. It should be pink to bright red and shiny. For the traditional
ileostomy, a tempo-rary plastic bag with adhesive facing is placed over the
ileostomy and firmly pressed onto surrounding skin. The nurse monitors the
ileostomy for fecal drainage, which should begin about 72 hours after surgery.
The drainage is a continuous liq-uid from the small intestine because the stoma
does not have a controlling sphincter. The contents drain into the plastic bag
and are thus kept from coming into contact with the skin. They are collected
and measured when the bag becomes full. If a continent ileal reservoir was
created, as described for the Kock pouch, continuous drainage is provided by an
indwelling reservoir catheter for 2 to 3 weeks after surgery. This allows the
suture lines to heal.
As
with other patients undergoing abdominal surgery, the nurse encourages those
with an ileostomy to engage in early am-bulation. It is important to administer
prescribed pain medica-tions as required.
Because
these patients lose much fluid in the early post-operative period, an accurate
record of fluid intake, urinary output, and fecal discharge is necessary to
help gauge the fluid needs of the patient. There may be 1000 to 2000 mL of
fluid lost each day in addition to expected fluid loss through urine,
perspiration, respiration, and other sources. With this loss, sodium and
potassium are depleted. The nurse monitors labo-ratory values and administers
electrolyte replacements as pre-scribed. Intravenous fluids are administered to
replace fluid losses for 4 to 5 days.
Nasogastric
suction is also a part of immediate postoperative care, with the tube requiring
frequent irrigation, as prescribed. The purpose of nasogastric suction is to
prevent a buildup of gas-tric contents. After the tube is removed, the nurse
offers sips of clear liquids and gradually progresses the diet. It is important
to immediately report nausea and abdominal distention, which may indicate
obstruction.
By the
end of the first week, rectal packing is removed. Because this procedure may be
uncomfortable, the nurse may administer an analgesic an hour before it is
performed. After the packing is removed, the perineum is irrigated two or three
times daily until full healing takes place.
PROVIDING EMOTIONAL SUPPORT
The patient understandably may think that everyone is aware of the ileostomy and may view the stoma as a mutilation compared with other abdominal incisions that heal and are hidden.
Because there
is loss of a body part and a major change in anatomy, the patient often goes
through the various phases of grieving—shock, disbelief, denial, rejection,
anger, and restitution. Nursing sup-port through these phases is important, and
understanding of the patient’s emotional outlook in each instance should
determine the approach taken. For example, teaching may be ineffective until
the patient is ready to learn. Concern about body image may lead to questions
related to family relationships, sexual function, and for women, the ability to
become pregnant and to deliver a baby normally. Patients need to know that
someone understands and cares about them. A calm, nonjudgmental attitude
exhibited by the nurse aids in gaining the patient’s confidence. It is
impor-tant to recognize the dependency needs of these patients. Their prolonged
illness can make them irritable, anxious, and depressed. The nurse can coordinate
patient care through meetings attended by consultants such as the physician,
psychologist, psy-chiatrist, social worker, enterostomal therapist, and
dietitian. The team approach is important in facilitating the often complex
care of this patient.
Conversely,
a surgical procedure to create an ileostomy can produce dramatic positive
changes in patients who have suffered from IBD for several years. After the
continuous discomfort of the disease has decreased and patients learn how to
take care of the ileostomy, they often develop a more positive outlook. Until
they progress to this phase, an empathetic and tolerant approach by the nurse
plays an important part in recovery. The sooner the patient masters the
physical care of the ileostomy, the sooner he or she will psychologically
accept it.
The
support of other ostomates is also helpful. The United Ostomy Association is
dedicated to the rehabilitation of osto-mates. This organization gives patients
useful information about living with an ostomy through an educational program
of litera-ture, lectures, and exhibits. Local associations offer visiting
ser-vices by qualified members who provide hope and rehabilitation services to
new ostomy patients. Hospitals and other health care agencies may have an
enterostomal therapy nurse on staff who can serve as a valuable resource person
for the ileostomy patient.
MANAGING SKIN AND STOMA CARE
The
patient with a traditional ileostomy cannot establish regular bowel habits
because the contents of the ileum are fluid and are discharged continuously.
The patient must wear a pouch at all times. Stomal size and pouch size vary
initially; the stoma should be rechecked 3 weeks after surgery, when the edema
has subsided. The final size and type of appliance is selected in 3 months,
after the patient’s weight has stabilized, and the stoma shrinks to a sta-ble
shape.
The
location and length of the stoma are significant in the man-agement of the
ileostomy by the patient. The surgeon positions the stoma as close to the
midline as possible and at a location where even an obese patient with a
protruding abdomen can care for it easily. Usually, the ileostomy stoma is
about 2.5 cm (1 in) long, which makes it convenient for the attachment of an
appliance.
Skin
excoriation around the stoma can be a persistent problem. Peristomal skin
integrity may be compromised by several factors, such as an allergic reaction
to the ostomy appliance, skin barrier, or paste; chemical irritation from the
effluent; mechanical injury from the removal of the appliance; and possible
infection. If irri-tation and yeast growth occur, nystatin powder (Mycostatin)
is dusted lightly on the peristomal skin.
CHANGING AN APPLIANCE
A
regular schedule for changing the pouch before leakage occurs must be
established for those with a traditional ileostomy. The patient can be taught
to change the pouch in a manner similar to that described in Chart 38-4.
The
amount of time a person can keep the appliance sealed to the body surface
depends on the location of the stoma and on body structure. The usual wearing
time is 5 to 7 days. The appli-ance is emptied every 4 to 6 hours or at the
same time the patient empties the bladder. An emptying spout at the bottom of
the ap-pliance is closed with a special clip made for this purpose.
Most
pouches are disposable and odor-proof. Foods such as spinach and parsley act as
deodorizers in the intestinal tract; foods that cause odors include cabbage,
onions, and fish. Bismuth sub-carbonate tablets, which may be prescribed and
taken by mouth three or four times each day, are effective in reducing odor. A
stool thickener, such as diphenoxylate (Lomotil), can also be prescribed and
taken orally to assist in odor control.
IRRIGATING A CONTINENT ILEOSTOMY
For a
continent ileostomy (ie, Kock pouch), the nurse teaches the patient to drain
the pouch, as described in Chart 38-5. A catheter is inserted into the
reservoir to drain the fluid. The length of time between drainage periods is
gradually increased until the reservoir needs to be drained only every 4 to 6
hours and irrigated once each day. A pouch is not necessary; instead, most
patients wear a small dressing over the opening.
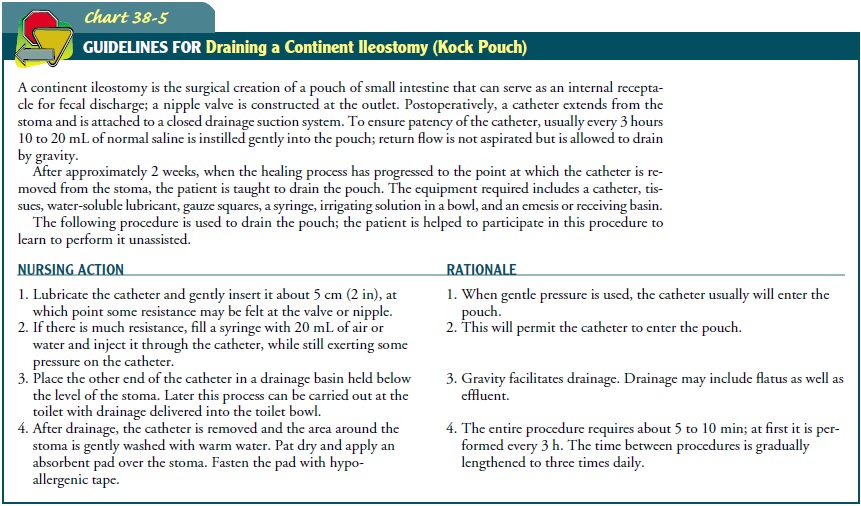
When
the fecal discharge is thick, water can be injected through the catheter to
loosen and soften it. The consistency of the effluent is affected by food
intake. At first, drainage is only 60 to 80 mL, but as time goes on, the amount
increases significantly. The internal Kock pouch stretches, eventually
accommodating 500 to 1000 mL. The patient learns to use the sensation of
pressure in the pouch as a gauge to determine how often the pouch should be
drained.
MANAGING DIETARY AND FLUID NEEDS
A
low-residue diet is followed for the first 6 to 8 weeks. Strained fruits and
vegetables are given. These foods are important sources of vitamins A and C.
Later, there are few dietary restrictions, ex-cept for avoiding foods that are
high in fiber or hard-to-digest kernels, such as celery, popcorn, corn, poppy
seeds, caraway seeds, and coconut. Foods are reintroduced one at a time. The
nurse assesses the patient’s tolerance for these foods and reminds him or her
to chew food thoroughly.
Fluids
may be a problem during the summer, when fluid lost through perspiration adds
to the fluid loss through the ileostomy. Fluids such as Gatorade are helpful in
maintaining the electrolyte balance. If the fecal discharge is too watery,
fibrous foods (eg, whole-grain cereals, fresh fruit skins, beans, corn, nuts)
are re-stricted. If the effluent is excessively dry, salt intake is increased.
Increased intake of water or fluid does not increase the effluent, because
excess water is excreted in the urine.
PREVENTING COMPLICATIONS
Monitoring
for complications is an ongoing activity for the pa-tient with an ileostomy.
Minor complications occur in about 40% of patients who have an ileostomy; less
than 20% of the compli-cations require surgical intervention (Kirsner &
Shorter, 2000).
Common
complications include skin irritation, diarrhea, stomal stenosis, urinary
calculi, and cholelithiasis. Peristomal skin irritation, the most common
complication of an ileostomy, re-sults from leakage of effluent. A pouch that
does not fit well is often the cause. The nurse or an enterostomal therapist
adjusts the pouch and skin barriers are applied. Diarrhea, manifested by very
irritating effluent that rapidly fills the pouch (every hour or sooner), can
quickly lead to dehydration and electrolyte losses. Supplemental water, sodium,
and potassium are administered to prevent hypovolemia and hypokalemia.
Antidiarrheal agents are administered. Stenosis is caused by circular scar
tissue that forms at the stoma site. The scar tissue must be surgically
released. Uri-nary calculi occur in about 10% of ileostomy patients because of
dehydration from decreased fluid intake. Intense lower abdominal pain that
radiates to the legs, hematuria, and signs of dehydration indicate that the
urine should be strained. Fluid intake is en-couraged. Sometimes, small stones
are passed during urination; otherwise, treatment is necessary to crush or remove
the calculi.
Cholelithiasis (ie, gallstones) occurs three times more com-monly in patients with an ileostomy than in the general population because of changes in the absorption of bile acids that occur post-operatively. Spasm of the gallbladder causes severe upper right abdominal pain that can radiate to the back and right shoulder.
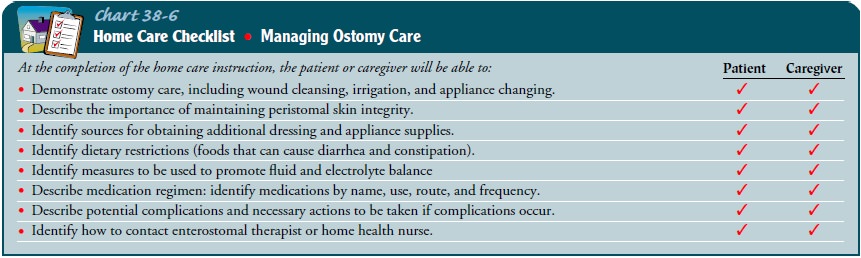
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
The
spouse and family should be familiar with the adjustment that will be necessary
when the patient returns home. They need to know why it is necessary for the
patient to occupy the bathroom for 10 minutes or more at certain times of the
day and why cer-tain equipment is needed. Their understanding is necessary to
reduce tension; a relaxed patient tends to have fewer problems. Vis-its from an
enterostomal therapy nurse may be arranged to ensure that the patient is
progressing as expected and to provide additional guidance and teaching as
needed.
The
patient needs to know the commercial name of the pouch to be used so that he or
she can obtain a ready supply and should have information about obtaining other
supplies. The names and contact information of the local enterostomal therapy nurse
and local self-help groups are often helpful. Any special restrictions on
driving or working also need to be reviewed. The nurse teaches the patient
about common postoperative complications and how to recognize and report them
(Chart 38-6).
Related Topics