Chapter: Medical Surgical Nursing: Management of Patients With Intestinal and Rectal Disorders
Appendicitis - Acute Inflammatory Intestinal Disorders
Acute Inflammatory Intestinal
Disorders
Any
part of the lower GI tract is susceptible to acute inflammation caused by
bacterial, viral, or fungal infection. Two such situations are appendicitis and
diverticulitis. These two conditions can lead to peritonitis, an inflammatory process within the abdomen.
APPENDICITIS
The
appendix is a small, finger-like appendage about 10 cm (4 in) long that is
attached to the cecum just below the ileocecal valve. The appendix fills with
food and empties regularly into the cecum. Because it empties inefficiently and
its lumen is small, the appendix is prone to obstruction and is particularly
vulnerable to infection (ie, appendicitis).
Appendicitis, the most common cause of acute abdomen
inthe United States, is the most common reason for emergency ab-dominal
surgery. About 7% of the population will have appen-dicitis at some time in
their lives; males are affected more than females, and teenagers more than
adults. Although it can occur at any age, it occurs most frequently between the
ages of 10 and 30 years (Yamada et al., 1999).
Pathophysiology
The appendix becomes inflamed and edematous as a result of either becoming kinked or occluded by a fecalith (ie, hardened mass of stool), tumor, or foreign body. The inflammatory process increases intraluminal pressure, initiating a progressively severe, generalized or upper abdominal pain that becomes localized in the right lower quadrant of the abdomen within a few hours. Eventually, the inflamed appendix fills with pus.
Clinical Manifestations
Vague
epigastric or periumbilical pain progresses to right lower quadrant pain and is
usually accompanied by a low-grade fever and nausea and sometimes by vomiting.
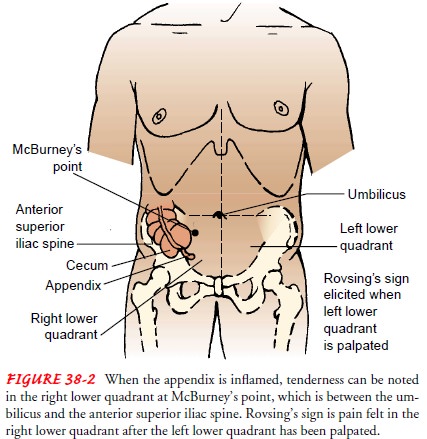
Loss of appetite is com-mon. Local tenderness is elicited at McBurney’s point
when pres-sure is applied (Fig. 38-2). Rebound tenderness (ie, production or
intensification of pain when pressure is released) may be pres-ent. The extent
of tenderness and muscle spasm and the existence of constipation or diarrhea
depend not so much on the severity of the appendiceal infection as on the
location of the appendix. If the appendix curls around behind the cecum, pain
and tender-ness may be felt in the lumbar region. If its tip is in the pelvis,
these signs may be elicited only on rectal examination. Pain on defecation
suggests that the tip of the appendix is resting against the rectum; pain on
urination suggests that the tip is near the bladder or impinges on the ureter.
Some rigidity of the lower por-tion of the right rectus muscle may occur.
Rovsing’s sign may be elicited by palpating the left lower quadrant; this
paradoxically causes pain to be felt in the right lower quadrant (see Fig.
38-2). If the appendix has ruptured, the pain becomes more diffuse; ab-dominal
distention develops as a result of paralytic ileus, and the patient’s condition
worsens.
Constipation
can also occur with an acute process such as ap-pendicitis. Laxatives
administered in this instance may produce per-foration of the inflamed
appendix. In general, a laxative or cathartic should never be given while the
person has fever, nausea, or pain.
Assessment and Diagnostic Findings
Diagnosis is based on results of a complete physical examination and on laboratory and x-ray findings. The complete blood cell count demonstrates an elevated white blood cell count. The leukocyte count may exceed 10,000 cells/mm3, and the neutrophil count may exceed 75%. Abdominal x-ray films, ultrasound studies, and CT scans may reveal a right lower quadrant density or localized distention of the bowel.
Complications
The major complication of appendicitis is perforation of the ap-pendix, which can lead to peritonitis or an abscess. The incidence of perforation is 10% to 32%. The incidence is higher in young children and the elderly. Perforation generally occurs 24 hours after the onset of pain. Symptoms include a fever of 37.7°C (100°F) or higher, a toxic appearance, and continued abdominal pain or tenderness.
Gerontologic Considerations
Acute
appendicitis does not occur frequently in the elderly popu-lation. Classic
signs and symptoms are altered and may vary greatly. Pain may be absent or
minimal. Symptoms may be vague, suggesting bowel obstruction or another
process. Fever and leuko-cytosis may not be present. As a result, diagnosis and
prompt treat-ment may be delayed, causing potential complications and
mortality. The patient may have no symptoms until the appendix ruptures. The
incidence of perforated appendix is higher in the el-derly population because
many of these patients do not seek health care as quickly as younger patients.
Medical Management
Surgery
is indicated if appendicitis is diagnosed. To correct or prevent fluid and
electrolyte imbalance and dehydration, anti-biotics and intravenous fluids are
administered until surgery is performed. Analgesics can be administered after
the diagnosis is made. Appendectomy (ie, surgical removal of the appendix) is
performed as soon as possible to decrease the risk of perforation. It may be
performed under a general or spinal anesthetic with a low abdominal incision or
by laparoscopy.
Nursing Management
Goals
include relieving pain, preventing fluid volume deficit, re-ducing anxiety,
eliminating infection from the potential or actual disruption of the GI tract,
maintaining skin integrity, and attain-ing optimal nutrition.The nurse prepares
the patient for surgery, which includes an intravenous infusion to replace
fluid loss and promote adequate renal function and antibiotic therapy to
prevent infection. If there is evidence or likelihood of paralytic ileus, a
nasogastric tube is inserted. An enema is not administered because it can lead
to perforation.
After
surgery, the nurse places the patient in a semi-Fowler position. This position
reduces the tension on the incision and abdominal organs, helping to reduce
pain. An opioid, usually morphine sulfate, is prescribed to relieve pain. When
tolerated, oral fluids are administered. Any patient who was dehydrated be-fore
surgery receives intravenous fluids. Food is provided as de-sired and tolerated
on the day of surgery.
The
patient may be discharged on the day of surgery if the temperature is within
normal limits, there is no undue discom-fort in the operative area, and the
appendectomy was uncompli-cated. Discharge teaching for the patient and family
is imperative. The nurse instructs the patient to make an appointment to have the
surgeon remove the sutures between the fifth and seventh days after surgery.
Incision care and activity guidelines are discussed; normal activity can
usually be resumed within 2 to 4 weeks.
If
there is a possibility of peritonitis, a drain is left in place at the area of
the incision. Patients at risk for this complication may be kept in the
hospital for several days and are monitored carefully for signs of intestinal
obstruction or secondary hemorrhage. Sec-ondary abscesses may form in the
pelvis, under the diaphragm, or in the liver, elevating the temperature and
pulse rate and increas-ing the leukocyte count.
When
the patient is ready for discharge, the nurse teaches the patient and family to
care for the incision and perform dressing changes and irrigations as
prescribed. A home care nurse may be needed to assist with this care and to
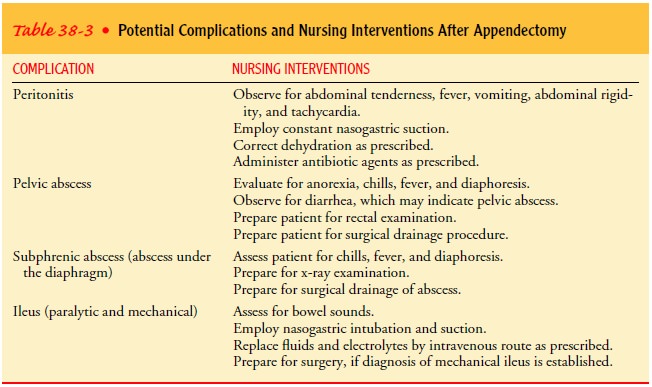
monitor the patient for com-plications and wound healing. Other potential
complications of appendectomy are listed in Table 38-3.
Related Topics