Chapter: Medicine Study Notes : Psychological Medicine
Treatment of Psychosis
Treatment of Psychosis
·
Early intervention improves
outcome, reduces disruption/trauma („collateral damage‟), etc. Important given
stage of life (adolescence) and the potential problems for subsequent social
and occupational development etc
·
Treatment programme involving
health professionals, family members, support agencies, and cultural/community
context
·
Brain‟s ability to process and
interpret information is affected Þ think carefully about how
information conveyed is received. Keeps the facts simple, avoid distractions
and pressure, ask one question at a time, give plenty of time to answer
·
Biological treatment: treat
early, immediately if psychotic, key issue with maintenance medication is
compliance
·
Psychological: supportive,
education, self-care skills. Social skills training and community integration
skills ® overcome withdrawal ® significant ¯ in readmissions
·
Social: assertive (to combat
stigma), community care
·
Relapse prevention: understanding
drugs, warning signs, prognosis, side effects
Antipsychotic Medication
·
= Neuroleptics or major
tranquillisers
·
May also use lithium,
carbamazepine, antidepressants and benzodiazepines for psychosis
·
Reduced risk of relapse in
schizophrenia, but 40% will still relapse within a year
·
Two effects:
o Reduces delusions and hallucinations (may take 1 –2 weeks)
o Tranquillising/calming effect (¯acute agitation, immediate
effect)
·
For first presentation, treat
with low dose and use atypicals (¯side effects ® compliance).
Use adjunctive long acting benzodiazepine for first few weeks to sedate and ¯agitation
·
Can be administered orally, IM,
IV and some as depot (but not yet for atypicals)
·
Side effects range over sedation,
extra-pyramidal, anti-cholinergic and hypotensive
·
All relatively effective at
reducing positive symptoms, but „atypicals‟ better than „typicals‟ at reducing
negative symptoms (eg ¯motivation, interest, lack of emotional display, restricted speech)
·
All have hepatic elimination
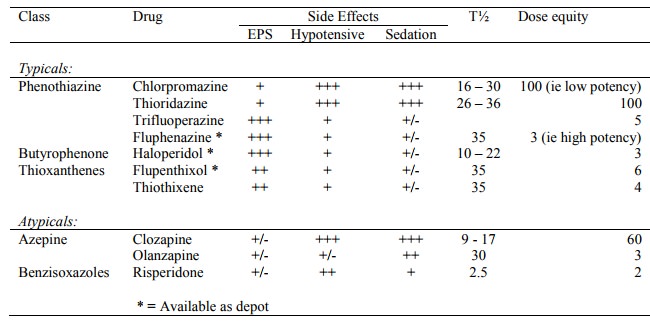
Typicals (ie Older antipsychotics)
·
Mode of action: block dopamine
(D2) receptors. Most also have low affinity for 5HT2 receptors. Varying amounts
of anticholinergic, antihistamine and anti a-1 effects
·
Adverse Effects:
o Extrapyramidal Syndromes (EPS):
§ Acute: Occur early in treatment – usually first two months.
§ Dystonias (muscle cramps and spasms): treat with benztropine parenterally
§ Akathisia (restlessness): treat with b blocker or benzodiazepine
§ Parkinsonism (tremor, cog wheel rigidity, bradykinesia, mask like face) – may improve with time
§ Anticholinergics only indicated in those whose antipsychotic dose cannot
be safely reduced. (= antiparkinsonian medication, eg antimuscarinic drugs such
as Cogentin)
o Tardive Dyskinesia:
§ Late onset dyskinetic syndrome due to antipsychotic drug treatment.
Usually months or years after treatment
§ Fairly common: 15 – 30%
§ Slow, repetitive involuntary movements of mouth/face, and maybe limbs
and trunk. Disappear during sleep
§ Risk factors: old age, organic brain disease, negative symptoms, alcohol
abuse
§ Irreversible in 50%
§ No established protocol for treatment: try dose reduction, lithium, or
change to clozapine
§ Made worse by dopaminergic agonists and anticholinergics
o Other effects:
§ Sedation
§ Anticholinergic effects (dry mouth, constipation, blurred vision, urinary hesitancy)
§ a blockade
(postural hypotension, tachycardia, delayed ejaculation)
§ Endocrine effects (PRL, marked weight gain, ¯libido, impotence, amenorrhoea)
o Neuroleptic Malignant Syndrome: Rare (0.2 – 1%) with hyperthermia,
rigidity, and impaired consciousness. 20% mortality. Emergency treatment
(cooling, fluids, etc)
·
Interactions:
o Potentiate sedation with hypnotics, alcohol, opioid analgesics
o Fluoxetine increases risk of EPS
Atypicals
·
Clozapine:
·
Mode of action: numerous
receptors: D1, D2, D4, 5HT2, blocks a-1, H1 and muscarinic receptors
o Effective in individuals not responsive to classical antipsychotics,
effective for positive and negative
symptoms, no extrapyramidal side effects, no impact on sexual or reproductive
function.
o Side effects:
§ Sedation, tachycardia, constipation, weight gain, and seizures (3% at highest dose)
§ Agranulocytosis/blood dyscrasias in 1-2 % by 1 year, most in first 18 weeks ® regular blood tests
§ Potent enzyme inhibitor: significant drug interaction potential
§ Serotonergic crisis with SSRIs
§ Hypersensitivity syndrome: PUO, arthritis, rash
§ Prolongation of QT
§ Myocarditis
·
Risperidone:
o Mode of action: binds to 5HT2 and D2 receptors, antagonises H and a-1 receptors
o Similar efficacy as other antipsychotics for positive symptoms. Effective for negative side effects and also affective symptoms (depression, anxiety).
o Some dose related extrapyramidal side effects. PRL at
high doses. Also insomnia, agitation, anxiety, headache
·
Olanzapine:
o Mode of action. Similar to clozapine.
Like clozapine has minimal impact on PRL
o Similar efficacy to haloperidol, but more impact on negative symptoms
o Sedation, headache, dizziness, constipation, dry mouth, weight gain
Related Topics