Chapter: Medicine Study Notes : Psychological Medicine
Alcohol Abuse
Alcohol Abuse
Safe Limits and Metabolism
·
Men and women have different
blood alcohol levels given the same dose due to lower Vd in women
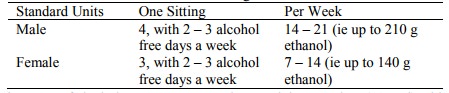
· Standard Unit = 10 g of alcohol. E.g. 1 can normal strength beer, 1 glass (120 ml) table wine, 1 glass sherry/port, 20 ml spirits (hotel nip)
·
Effects (if no tolerance):
o 50 mg: relaxation, emotional liability
o 100 mg: judgement affected, reactions slow
o 150 mg: amnestic blackouts (can‟t remember afterwards)
o 200 mg: ataxia, vomiting, nystagmus, drowsiness
o 350 mg: coma, respiratory depression, death
o Intoxication can be life threatening
·
Driving:
o Legal blood limit = 80 mg/100ml (17.4 mmol/L)
o Legal breath limit = 400 mg/L breath
o Driving skills impaired from 40 – 50 mg/100 ml
·
Metabolism:
·
10 g per hour, zero order
kinetics
·
= 15 – 20 mg/100 ml blood/hour (3
– 4 mmol/hr) = one standard drink
· Twice this rate of clearance with chronic alcohol consumption, less in liver disease
·
Alcohol changes NAD/NADH ratio ® alters
redox potential ® widespread effects (eg lipids, ¯sugars, etc)
Classifying alcohol use
·
Alcohol Dependence: need to drink every day
o Important features:
§ Tolerance: due to pharmacodynamic and pharmacokinetic (eg enzyme
induction) processes
§ Cross-tolerance, eg alcohol and BZDs
§ Physical dependence: Withdrawal syndrome on abstinence
§ Psychological dependence: Emotional need to compulsively take a drug (even if no physical withdrawal syndrome)
o Characterised by: tolerance (CNS adaptation and pharmacokinetic), narrowing of drinking pattern (stereotyped drinking), amnesic blackouts, withdrawal symptoms, awareness of loss of control, failed attempts at abstinence, preoccupation with drinking, drinking to relieve withdrawal symptoms
o Look for: compulsive binges with frequency, stereotyped drinking, intake over 60 g ethanol/day, chronic social and health problems, neurological problems
o Use CAGE questions to assess dependency: Have you ever tried to Cut Down, Annoyed by others telling you to cut down, Guilt, Eye-opener
·
Hazardous Drinking.
Heavy drinking with no “obvious” problem
o Characterised by prolonged (eg 5 years or more), regular (eg almost
daily, or weekend binges), excessive consumption with a high risk of physical
mental and social implications, but no dependency features – but maybe some tolerance
and occasional amnesic blackouts, may not be associated with acute intoxication
o Look for: episodic heavy social drinking to intoxication, increasing psychosocial problems, accidents, inflammation of stomach, liver, pancreas
·
Problem Drinking: problems related to alcohol
without dependency and with or without excessive regular consumption. May result from isolated acute intoxication
or drinking with medical contraindication – injury, aggression, binge drinking,
family, financial, occupational problems
·
Remember: Drug abusers often
abuse multiple drugs (eg alcohol, BZDs, and marijuana)
Assessment
· For liver and pancreatic effects see Topic: Alcoholic Liver Disease
·
Differential of drowsiness/confusion
in alcoholic:
o Alcohol intoxication
o Sedatives
o Post-ictal (eg seizures with alcohol withdrawal)
o Wernicke‟s encephalopathy
o Subdural haematoma: grow slowly, compounded by global atrophy due to
alcohol
o Hepatic encephalopathy
o Alcoholic hypoglycaemia
· Assessment of co-existing disease is vital:
o Other drug use (BZD, sedatives, opioids ® also
have withdrawal features)
o Primary depressive disorder (in addition to alcohol-induced depression
which resolves quickly)
o Gastro disorders: oesophagitis, pancreatitis, liver disease, small bowel
dysmotility
o Respiratory: Obstructive sleep apnoea, aspiration pneumonia, TB
o Musculoskeletal: chronic proximal myopathy, osteoporosis
o Carcinomas: larynx, oesophagus, lung
o Neurological: peripheral neuropathy, dementia, cerebellar atrophy,
Wernicke-Korsakoff syndromes, Head injury (subdural haematoma), haemorrhagic
stroke
o Cardiovascular: arrhythmias, congestive cardiomyopathy, hypertension
o Blood and nutritional: macrocytosis, folate and iron deficiency,
impaired leucocytes, hypocalcaemia, hypokalaemia, electrolyte disturbances
·
Investigations:
o Alcohol levels
o LFT
o FBC (anaemia)
o Glucose (® ?hypoglycaemic)
o Coagulopathy: INR
o Other drugs, eg BZD
Pathological Effects of Alcohol on the Brain
·
Cerebral atrophy:
o Common. Seen in over ¼ of long
term alcoholics at post-mortem
o Ventricular dilation, widening of the cerebral and cerebellar sulci
o No specific cortical changes have been described. No classical changes of multi-infarct dementia or Alzheimer‟s
· Wernicke-Korsakov Syndrome:
o Due to ¯Vitamin B1 (Thiamine) – Marmite and Cereals are good sources
o Thiamine is not stored in the body, signs of deficiency can appear
within a month – especially in beer drinkers (high carbohydrate intake ® thiamine
requirement)
o Rare triad of:
§ VI nerve palsy (®vertical/horizontal nystagmus)
§ Ataxia (vestibular dysfunction)
§ Confusion
o Pathology:
§ Acute: petechial haemorrhages in the grey matter surrounding the third
and fourth ventricles and aqueduct
§ Chronic: shrinkage and haemosiderin staining (especially of mamallory
bodies)
o If prolonged leads to Korsakov‟s amnesic psychosis
·
Vitamin B12 (cobalamin)
deficiency:
o Leads to:
§ Peripheral neuropathy, demyelination and degeneration of the posterior
and lateral columns of the spinal cord
§ Variety of confusional, amnestic and psychotic alterations
Treatment of alcohol abuse
·
Drug treatment of alcohol abuse:
o Effects of chronic alcohol:
§ Dopamine
activity
§ Opioid activity (Þ ?naloxone/naltrexone ® ¯craving)
§ Sensitivity
to GABA
§ ¯Serotonin
activity
o Ie, lots of potential neurotransmitter targets in reward pathways to ¯cravings,
etc
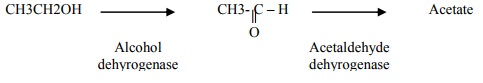
o Antabuse (disulphram):
§ Blocks second step of metabolism pathway ® acetaldehyde ® flush, vomiting, ¯BP
§ Takes 12 hours to block enzyme system. Has effect within ½ hour of a
drink (one drink is enough)
§ Contraindications: heart disease (can‟t cope with ¯BP), makes depression/psychosis worse
§ Administration needs to be supervised: if taken at own discretion then little impact on abstinence
o Acamprosate (Campral): ¯craving, must be taken 3 times daily (a pain!), start 7 days post detox.
Not in elderly, pregnant, liver or renal disease. No hypnotic, anxiolytic or
antidepressant effects
· For non-drug treatment, see Topic: Treatment of Substance Abuse
Alcohol Withdrawal
·
Most common drug withdrawal
state. Can be life threatening (unlike
opioid withdrawal)
·
Detoxification is only the first
step in treatment
·
Aetiology of alcohol withdrawal
syndrome poorly understood
·
Features of withdrawal:
o A spectrum. Delirium Tremens describes severe withdrawal only
o Minor withdrawal (peaks at day 2): restlessness, anxiety, nausea, disordered sleep, headache, tachycardia, hypertension, tremor
o Major withdrawal (peaks at day 5): Agitation, behavioural disorders, confusion, sweating, fever, paranoia, hyperventilation
o Seizures: if they occur, are most likely on day 1 – 3, usually only one, usually grand mal, status rare
o Hallucinations: usually visual (auditory unlikely), on day 2 – 4
· Management:
o Get pre-detoxification blood alcohol level. Helps with assessment (how tolerant are they?). Avoid too much sedative if high. Alcohol metabolised at 20 mg/dl/hour (4 mmol/L/hour) – can predict when it will reach zero
o Previous withdrawal severity good indicator of likely current severity. Other indicators of severity: > 15 standard drinks a day, early morning drinking, hypokalaemia, intercurrent illness
o If likely to be severe, or if co-existing medical, psychiatric illness or other addiction, withdrawal should be medically supervised (ie admit them). Mattress on the floor with constant nursing attention. If dehydration or constant sweating then iv fluids
o Otherwise at home or outpatients if good social support
o Routine blood tests: FBC, ESR, U+E, B12/folate, LFT, AST, GGT, PT, BS
o Parental thiamine followed by short oral course (25 mg po twice daily)
o Treat withdrawal with drugs which have cross-tolerance with alcohol (ie
BDZs) once they’re no longer intoxicated
o Use BZDs or chlormethiazole
§ Give sedatives with extreme caution if measurable blood alcohol levels
§ Diazepam 10 – 20 mg/4 hourly for moderate withdrawal, 20 mg/2 hourly iv
for severe. Resist protracted sedatives, otherwise ®
addiction. If liver disease then reduce dose
§ Oral chlormethiazole 1 gm 6 hourly
o Additional treatments:
§ b blockers
for tremor, hypertension (except if CORD or CV disease).
§ Haloperidol 1 – 5 mg 6 hourly if hallucinations
§ Sodium Valproate (Epilim) 600 mg stat po, then 400 mg 8 hourly for 5 days, if history of seizures – care if liver disease. Likely to occur early in withdrawal, especially if history of seizures with previous withdrawal
Related Topics