Chapter: Medicine Study Notes : Psychological Medicine
Anxiety Disorders
Anxiety Disorders
Introduction
·
Anxiety is usually normal, useful
and protective. We learn to fear normal anxiety. Yerkes Dobson Curve (1908):
moderate levels of anxiety can improve performance, but performance improvement
plateaus and then falls with anxiety. Anxiety becomes debilitating if severe
· 4 clusters of responses:
o Physiological: autonomic nervous system arousal, ¯sleep
o Cognitive: perception of danger, threat, loss, hypervigilence
o Affective: nervousness, fear, ¯concentration
o Behavioural: fight or flight
·
Anxiety disorders lead to:
o Over activation of cognitions about personal danger
o Underestimation of ability to cope
·
Differential Diagnoses:
o Exclude anxiety due to substance intoxication or withdrawal, or due to delirium
o Physical conditions that cause or exacerbate anxiety (hyperthyroidism, hyperventilation – eg asthma, phaeochromocytoma, drug withdrawal, etc)
·
Becomes a disorder when it causes
significant distress or interferes with social or occupational functioning
History Taking in Anxiety Disorders
·
Introductory Questions:
o Are there currently things in your life that are causing distress/worry?
o Are there things that have happened in the past that you can‟t stop
thinking about?
o How is your general health?
o Any one else in your family had similar problems?
o Most anxiety is part of a mixed anxiety/depression ®
importance of full psychiatric assessment
· General Anxiety
o Would you describe yourself as a worrier? Do you worry about things that
others don‟t worry about?
o Do you sometimes make mountains out of molehills?
o Do you every find it hard to make decisions?
·
Panic
o Have you ever felt your heart pounding, felt frightened/afraid – what do
you think was the cause?
o Ever felt like a disaster was about to happen to you?
o Do they occur when other people wouldn‟t feel afraid?
o Do you avoid going out?
· Phobias/Avoidance:
o Is there anything you would avoid if you could? What happens if you are unexpectedly faced with that object/situation?
o Do you have worries/fears that prevent you from doing things you would
like – or that others can do without difficulty?
o Are you only worried if others will see you?
o Are you worried/anxious in other settings?
· Obsessions and Compulsions:
o Obsessive thoughts: Any thoughts that keep coming repeatedly into mind,
even when you‟re trying to get rid of them?
o Compulsive rituals:
§ Do you ever have to repeat actions over and over which most people would
only do once?
§ Do you ever find yourself having to do things over and over again to get them just right?
§ Do you find yourself spending a lot of time doing things like cleaning
or checking that everything is safe?
§ What happens if you are interrupted when doing these things?
·
Trauma:
o Do you still have recurrent memories of an upsetting event?
o Do you have nightmares, have trouble sleeping, or feel jumpy?
o Are there things that remind you of the event? Do you avoid these?
·
How has the trauma changed the
way you feel about the future, about what you enjoy?
Panic Disorder (with or without agoraphobia)
·
Panic attack:
o = Intense exacerbation of autonomic responses: discrete episode of
intense dread, fear or doom
o Sudden, abrupt onset
o Symptoms include racing heart, trembling, SOB, nausea, fear of dying or losing control, going crazy. May have limited symptom attacks
o Found across anxiety disorders and in non-anxious population
· Panic Disorder:
o Recurrent and unexpected panic attacks. Situationally-bound panic attacks are characteristic of social or specific phobias, although situationally-predisposed panic attacks are frequent in Panic Disorder
o Catastrophic misinterpretation of bodily sensations/mental events (eg
has palpitations and thinks they‟re having a heart attack). Normal bodily
sensations misinterpreted
o High anticipatory anxiety: persistent worry about having additional
attacks
o Hyper-vigilance for feared sensations
·
Agoraphobia:
o = „Fear of fear‟
o Fear of situation where escape may be difficult or embarrassing in the
event of a panic attack
o Avoid or endure with dread situations associated with panic attacks and feared bodily sensations
o Characteristically involve clusters of situations including being
outside the home, being in a crowd, on a bridge, in a car, train or bus
o But fear NOT of the situation
o Can occur with or without a history of panic disorder
o In Panic disorder, the more agoraphobic avoidance there is, the worse the prognosis
·
Differentiating from Social
Phobia: in panic disorder, fear evaluation of what panic causes them to do
(difficulty breathing, dizziness, weakness in limbs). In Social phobia, fear
evaluation of what they do or say regardless of panic (blushing, sweating,
trembling)
Specific Phobia
·
Persistent and irrational fear
and avoidance of a specific object or situation
·
Leads to avoidance or intense
anxiety on exposure to feared stimulus
·
Fear recognised as excessive
·
Disruptive to functioning
(important – who cares about a snake phobia in NZ)
· Can also be anxious about fear reaction
·
Usually related to animals (mice,
snakes, spiders), natural environment (earthquakes), blood, injection or
injury; specific situations (eg claustrophobia)
·
Develop due to:
o Direct conditioning through personal experience
o Verbal or vicarious transmission (eg develop shark phobia after watching
Jaws)
·
Treatment:
o Graded exposure
o Cognitive restructuring
o Physiological control: relaxation and medication (short-term only)
Social Phobia
·
Fear of negative evaluation of
performance in social situations. Fear they will do or say something
embarrassing or humiliating. Fear visible anxiety symptoms
·
Probability and cost of negative
evaluation is over-estimated
·
Early onset
·
Leads to avoidance of social
gatherings, public travel, etc
·
Epidemiology: 6 month prevalence
is 2 per 100, more females, onset in teens through to 35 ® social
isolation
·
Aetiology: ?conditioned response,
genetics
Generalised Anxiety Disorder
·
Worry about worry: a meta-worry!
·
Excessive and persistent worry
about a number of areas of life including family, health, job, finances, etc
·
Worrying dominant source of discomfort:
spend half an average day worrying – most recognise they worry excessively
about minor things but can‟t control it
·
At least six-month duration,
chronic fluctuating course
·
Epidemiology: 2 – 8 % of the
population, onset 20 – 40 years, male = female
·
Symptoms: restlessness, feeling
on edge, difficulty concentrating, mind going blank, irritability, muscle
tension, sleep disturbance (esp difficulty getting back to sleep after waking,
anticipatory thoughts while awake)
·
Co-morbidity/differential: mood
disorders, adjustment disorder (clearly identifiable stressor), panic attacks,
socially anxious, low self-esteem, avoidant or dependent personality disorder
·
Treatment:
o Education
o Training: relaxation, breathing control, structured problem solving, gradual confrontation of fears
o Avoid sedatives: they will love them but will become dependent on them
and underlying problems won‟t be fixed
o Specialist referral if symptoms persist for a further 3 months
Obsessive Compulsive Disorder
·
Upsetting and intrusive obsessional
thoughts that are difficult to control (e.g. fear of contamination), leading to
compulsive rituals (although can have rituals in the absence of obvious
obsessions)
·
Common compulsions: cleaning,
checking, counting
·
Treatment:
o Hard to treat with CBT and antianxiolytics
o Consider antidepressants
o Some evidence of effectiveness of low dose respiridone (?may be
delusional component)
Post Traumatic Stress Disorder (PTSD)
·
Long lasting anxiety or memories
about a severe traumatic event, including nightmares, flashbacks, anxiety,
avoidance of reminders
· Diagnostic criteria:
o Actual or threatened severely traumatic event where the response was intense fear, helplessness or horror
o Event is persistently re-experienced: recollections, dreams, distress to cues of an aspect of the event
o Persistent avoidance of stimuli associated with the trauma (triggers) and numbing of general responsiveness (eg ¯interest in activities, detachment, etc)
o Persistent symptoms of increased arousal (eg difficulty sleeping, irritability, ¯concentration, hypervigilance)
o Duration of > 1 month
o Causes significant distress or impairment in social/occupational
function
·
Types:
o Acute: duration of symptoms < 3 months
o Chronic: duration of symptoms > 3 months
o Delayed onset: onset > 6 months after stressor
·
Differential: OCD, Acute stress
disorder (resolves within 4 weeks), adjustment disorder, psychotic disorders,
malingering
Acute Stress Disorder
·
Distinguished from PTSD by
duration < 1 month (i.e. short term reaction). Includes avoidance, fear of
being alone, muscle tension, disbelief, problems with sleep, concentration and
memory, guilt, self-doubt
Treatment of Anxiety Disorders
Cognitive Behavioural Therapy (CBT)
·
Effective for most anxiety
disorders
·
Response more long lived than for
drug treatment
·
Includes: breathing retraining,
deconditioning, cognitive restructuring, relaxation, graded exposure,
desensitisation
Psychodynamic Psychotherapy
·
Symptoms result from mental
processes outside conscious awareness.
Aim is to elucidate these
·
Identify and alter core conflicts
Drug Treatment
·
Benzodiazepines: may be useful
for the short term or acute treatment of acute stress reactions. Due to
tolerance and dependence, these are not useful for long-term use
·
Antidepressants:
o For severe panic disorder (with or without agoraphobia), TCA‟s (eg
imipramine) are the medication of choice. Suppression of panic attacks may
occur after 4 – 6 weeks. Minimum treatment usually 6 months. Maximum is 18
months. Use alternative therapies if it fails after this time
o For OCD, clomipramine (a TCA) and SSRIs may be a useful adjunct to CBT.
Help minimize compulsions and manage the depression often associated with OCD.
·
Betablockers: Useful for the
treatment of social phobia when performance anxiety is the main problem. These
prevent noticeable symptoms (eg blushing or shaking), which are typically
interpreted catastrophically by individuals. However, these drugs are not
useful if the anxiety is more generalized
Benzodiazepines
·
Mode of action: enhance GABA
inhibition throughout the CNS
·
GABA (gamma-amino-butyric acid)
increases membrane Cl- permeability ® hyperpolarisation
·
Binding affinity important in governing
duration and degree of effect, in addition to elimination and dosage.
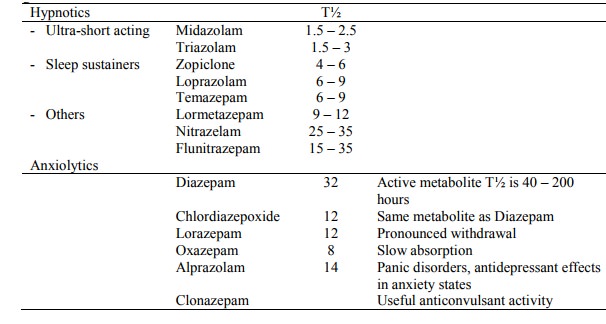
· Key pharmacodynamic differences:
o Chlordiazepoxide and Diazepam: shorter elimination time than their
active metabolites. Doses of benzos with active metabolites should be reduced
in the elderly, especially if ¯renal function
o Midazolam: often used as premed for procedures and GA – relaxes and amnesia
o Zopiclone (Imovane): differs from BDZs and barbiturates, but has same
actions (sedation, anticonvulsant, anti-aggressive and muscle relaxant). Binds
to BDZ binding sites. Peak plasma conc. in 1 hour, T½ of 4 hours. At higher
doses: hangover effect, memory disturbance, rebound insomnia, interaction with
alcohol
· Metabolism:
o Eg: diazepam ® temazepam ® oxazepam
o Inactive conjugates excreted
· Adverse Effects:
o Daytime sedation: with long acting BDZs where slow elimination leads to
accumulation of drug and active metabolites
o Daytime agitation/irritability: with ultra short acting BDZs (triazolam,
midazolam), especially in those with anxiety
o Psychomotor functional impairment: beware if driving or operating
machinery
o Amnesia: with short acting BDZs
o Physical dependence: All BDZs are addictive
o CNS effects of BDZs all exacerbated by alcohol
o Broken sleep patterns are particularly common after withdrawal of hypnotics
o Discontinuation of long-term use must be gradual (2 – 3 months) never
abrupt. Withdrawal similar to hyperadrenergic state – anxiety, tremor, ataxia,
confusion, insomnia, nausea, seizures (especially with lorazepam). Withdrawal
syndrome can be prolonged (ie months). Treating withdrawal: change to diazepam
(greater dose flexibility), reduce dose by 10% every 2 – 4 weeks. Use
counselling and relaxation
·
Lorazepam as a hypnotic where
insomnia is a complication of anxiety – but never just as a hypnotic
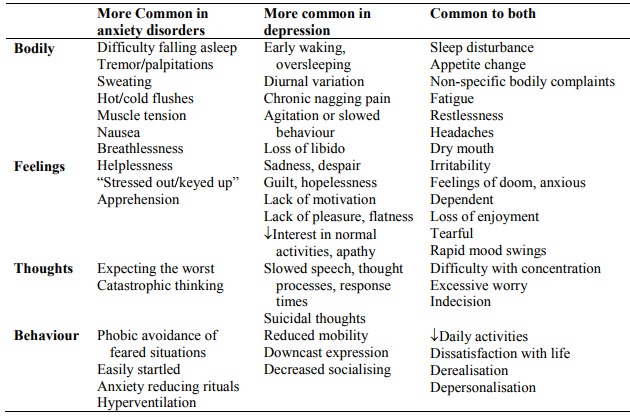
Differentiating Anxiety and Depressive Symptoms
· Coexistence of anxiety and depressive symptoms is common:
o Depressive symptoms occur secondarily especially in panic disorder, agoraphobia and OCD. If anxiety disorders go untreated ® demoralised and progressive restrictions on function ® depression
o Anxiousness and irritability are seen in the majority of depressed
patients, panic attacks may occur
·
Differentiating:
o GAD/Panic disorder don‟t usually have full range of vegetative symptoms
o Anxious patients have trouble getting to sleep, depressed wake early
o Anxious patients don‟t loose the capacity to enjoy things or be cheered
up
o Asking which symptoms came first can be helpful
Related Topics