Chapter: Medicine Study Notes : Psychological Medicine
Depressive Mood Disorders
Mood Disorders
Depressive Disorders
·
References: Guidelines for the
Treatment and Management of Depression by Primary Healthcare Professionals,
National Health Committee, September 1996
Diagnosis of Major Depressive Disorder/Episode (MDE)
·
Handy pneumonic:
o S: Sleep
o A: Appetite and weight
o D: Dysphoria and anhedonia
o F: Fatigue
o A: Agitation/retardation
o C: Concentration
o E: Esteem
o S: Suicide
·
DSM IV criteria:
o 5 or more of the following present during the same 2-week period and
represent a change from previous functioning. At least one symptom must be
depressed mood or loss of interest/pleasure [NB exclude symptoms clearly
related to a general medication condition, delusions or hallucinations]. Note
duration and persistence of each symptom, and compare to normal:
§ Depressed mood, most of the day, nearly every day (either self report or observed by others)
§ Markedly diminished interest or pleasure in all, or all most all, activities (exclude grief reaction)
§ Significant weight loss/gain or ¯/ in
appetite (exclude cancer, Tb, hypothyroid)
§ Insomnia/hypersomnia nearly every day (exclude sleep apnoea)
§ Psychomotor agitation or retardation (excessive repetitious and pointless motor activity that is associated with feelings of tension. Needs to be observable, not just felt). Eg have you been fidgety/restless or felt „stuck in the mud‟ or in slow motion?
§ Fatigue or loss of energy nearly every day
§ Feelings of worthlessness or excessive or inappropriate guilt nearly
every day. Eg how do you feel about yourself, have you blamed yourself for
things, do you feel guilty?
§ Diminished ability to think or concentrate, or indecisiveness, nearly
every day
§ Recurrent thoughts of death, suicidal ideation without a plan, an
attempt or a plan
o Symptoms do not meet criteria for a mixed episode
o Symptoms cause significant distress or impairment in social and
occupational functioning. Eg what difficulties have all these symptoms caused?
o Exclude depression if symptoms:
§ Are due to physical illness, medication or street drugs
§ Occur within 2 months of significant bereavement (except if marked
impairment, morbid preoccupation with worthlessness, suicidal ideation,
psychotic symptoms or psychomotor retardation). Key difference between grief
and depression is whether they themselves feel worthless or not
· Also review risk factors:
o Prior history of major depressive episode or suicide attempt. Previous episode ® 50% lifetime risk of recurrence
o Family history of mood disorder or suicide attempts. If no family history then lifetime risk 10 – 20%. If heavy genetic loading this may double the risk (very polygenic)
o Chronic or severe physical illness (may ® demoralisation
and hopelessness)
o Concurrent substance abuse
o Recent stressful life events and lack of social support (stress should not be used to „explain away‟ symptoms, stress may precipitate a major depressive episode)
o Childhood trauma, abuse, parental conflict or deficient parental care
o Recent childbirth or other family changes (eg divorce, children leaving
home)
o Responsibilities for caring for others (eg elderly relatives)
·
Differentials:
o Substance abuse
o Other psychiatric disorders, eg anxiety, eating and adjustment
disorders, personality disorders, somatization
o Dementia in older people (a key differential is memory)
o General medical conditions and medication. Drugs affecting mood:
§ Steroids: on 20 mg 1.3% get depression, on 80mg 20% get depression
§ Lipid soluble b blocker
§ New drug affecting P450 metabolism and plasma
conc. of existing drug
o Grief reaction. Depressive symptoms common during periods of grief.
Usually begins within 2 – 3 weeks of bereavement and usually resolves without
treatment – although supportive counselling/practical help may be indicated
·
In children and adolescents,
feelings of guilt, emptiness, self-dislike and failure are common – but are
underreported by parents, who may instead report a decline in behaviour or
academic performance
·
Can use questionnaires: e.g. GHQ
(General Health Questionnaire) or CES-D – useful either for screening or in
borderline situations – gives something to discuss with patient
·
Little point in trying to
separate exogenous from endogenous depression (often a chicken & egg
situation). It‟s usually multifactorial – regardless of cause may well need a
multi-factorial approach to management
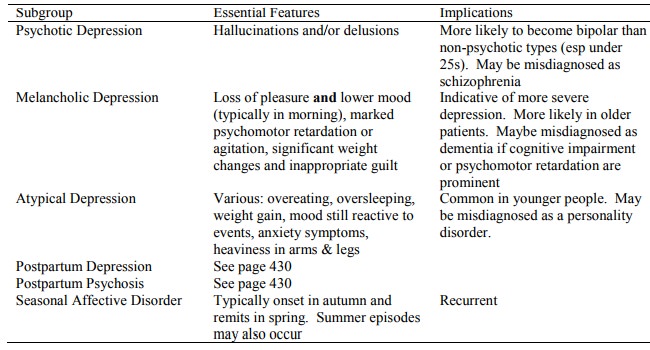
Subgroups
Epidemiology and Aetiology
·
Lifetime risk of depression in
women is 20%
·
Female: Male is 2:1, but in
younger cohorts an in male depression is bringing the ratio down to 1.6:1. This is not an
artefact of help-seeking behaviour
·
Rate is increasing
·
Variety of theories:
o Biological (eg neurotransmitter dysfunction)
o Freud: unresolved early childhood events resurrected by similar events
in later life
o Bent (?): Cognitive triad: people feel helpless ® hopeless
® worthless. Selective abstraction
–
o extrapolate from one event to everything. Treatment: Uncover underlying
schema. Then challenge faulty thinking (is it always that bad?), challenge
automatic thoughts
Assessment
·
Cultural issues:
o Different cultures have different views on the cause and treatment of
depression.
o Appreciating the cultural perception of the individual ® better
therapeutic relationship and effectiveness of intervention.
o Consider referral to culturally appropriate service.
o Cultural issues may affect the way the interview is conducted. Eg if
Maori, establish initial rapport before asking name and personal information,
don‟t make eye contact when discussing sensitive information, a family member
speaking on a patient‟s behalf is not being dominating, etc
·
Assessment of severity: Use the
number of DSM IV criteria met or severity rating scales. Allows classification
into mild, moderate and severe. Can be used to monitor progression of treatment
and relapse
·
Assess duration: (> 6 months,
> 24 months)
·
Refer to specialist services
when:
o There is serious risk of suicide (or harm to others, especially younger
children)
·
The child is under the age of 13
years
·
There are psychotic symptoms or
bipolar disorder (depressed phase)
· The diagnosis is unclear and needs further evaluation
·
Melancholic features are so
severe that they are unable to look after themselves and have inadequate
community support
·
There are complex problems (eg
poor relationship, another psychiatric disorder)
·
Considering enhancing
antidepressants with mood stabilisers (eg lithium)
·
Failure to respond to recommended
treatment within 12 weeks
Treatment of Major Depressive Disorder
·
Fundamental to treatment is:
o Establishing positive therapeutic relationship
o Developing shared understanding of problems
·
Safety: suicide risks common
(lifetime risk 25 – 50%). Higher in delusional Major Depressive Episode.
Consider safety of others, especially if psychotic beliefs or Postpartum
Depression
·
Lifestyle changes that have been
shown to be effective: stress management, ¯alcohol and drugs, good sleep
patterns, a balanced diet, and physical exercise
·
Role of family, friends and self
help groups important in maintaining a supportive environment
·
Education (over time):
o Depression is an illness not a weakness.
o Treatment is effective and recovery is normal.
o Recurrence is possible so compliance is important. However, sometimes
there is only partial remission between episodes. Recognition of warning signs
and seeking early treatment will reduce severity
·
Psychological treatment:
o Indicated if:
§ Person with mild to moderate chooses this as first line
§ If partial response to drugs at week 6 or 12 and residual symptoms are largely psychological
§ There are continuing issues/cognitive beliefs that the risk
of relapse
§ Not as sole treatment in severe, psychotic or melancholic depression
o Promoting change: behaviour, thoughts, emotion
o Different therapies:
§ Cognitive behavioural therapy (See Topic: Cognitive Behavioural Therapy (CBT)
§ Problem solving therapy (See Topic: Problem Solving Therapy)
§ Interpersonal therapy
§ Hypnotherapy
§ Psychoanalysis
§ Transactional analysis
§ Martial or family therapy
· Drug treatment: See Topic : Antidepressant and Mood Stabilising Medication
·
Electroconvulsive Therapy (ECT):
o Relieves symptoms is 80% of all severe depressions (not just those
resistant to medication)
o Indications:
§ Psychotic depression
§ Depressive stupor (severe psychomotor depression)
§ Severely suicidal
§ Previous good response to ECT
o Risks: little risk of brain injury – risks are those of a general anaesthetic. Most troubling side effect is memory loss. Anteriograde loss is usually short lived. Some retrograde loss may be permanent
o Response is proportional to length and quality of seizure. Usual course
is about 6 cycles. If no response after 12 cycles then stop
o Also need to establish on an antidepressant that they haven‟t failed on
·
Monitoring treatment in primary
care:
o Check for treatment response, side effects, and alteration in stressors
or supports
o If severe, monitor twice weekly by consultation and phone, if mild then
weekly
o Assess response in week 6
Related Topics