Chapter: Medicine Study Notes : Psychological Medicine
Postpartum Mood Disorders
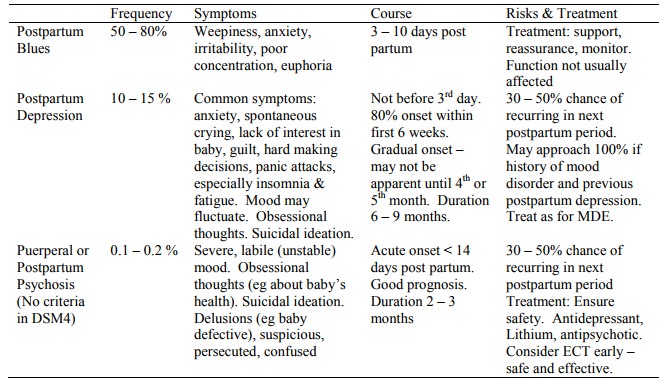
Postpartum Mood Disorders
·
Screen at post-natal check up (6
weeks) using Edinburgh Postnatal Depression Scale (EPDS), but still needs
careful clinical assessment
·
Differential: hypothyroidism
(more common post-partum), recurrence of previous psychiatric illness, initial
presentation of a psychiatric illness (eg schizophrenia or anxiety disorders –
postpartum period increases risk), adjustment disorder with depressed mood
·
Possible aetiological factors:
o Stress of delivery, difficult pregnancy
o Lack of sleep
o Hormonal
o Isolation, lack of support
o Internal conflicts about role as mother: motherhood idealised or
devalued, very difficult adjustment in role, powerless, dependent, alone, may
have had unrealistic expectations, etc
o May not have wanted to be pregnant, may now feel trapped in unhappy situation (eg relationship)
o Cultural factors: cultures vary in support offered (eg by extended
family) to new mother, in pressures to return to work (variable maternity leave
policies), differing attitudes to female children, etc.
·
Considerable overlap in the risk
factors for major depression, post-partum depression, inadequate parenting and
child abuse
·
Treatment:
o Check whether drugs enter breast milk.
o Indications for antidepressants similar for those for other mood disorders
o If agitated or anxious, more sedating antidepressants are appropriate
(eg imipramine) or even small doses of antipsychotics
·
Long term effect of postnatal
depression on child development: disturbances in mother-infant relationships
(eg attachment), impaired cognitive and emotional development in later infancy,
and risk of longer-term behavioural and social development of the child.
These factors compounded by indices of socio-economic adversity, which are risk
factors for these outcomes and for depression. So good initial diagnosis and
treatment important
Related Topics