Chapter: Medicine Study Notes : Psychological Medicine
Personality Disorders
Personality Disorders
Diagnosis
· Personality disorder =
o An enduring pattern of inner experience and behaviour that deviates
markedly from the expectations of the individual‟s culture
o Is inflexible and pervasive across a broad range of situations
o Has its onset in adolescence or early adulthood, is stable over time and leads to distress
o And is manifested in two or more of the following: interpersonal
functioning, affectivity (emotionality), impulse control, cognition (style of
thinking)
·
Key characteristics:
o Rigidity: very pervasive rigidity of cognitions and behaviours
o Avoidance: don‟t want to look at or experience their thoughts or feelings ® problem for therapy (compulsory treatment won‟t change anything)
o Long-term interpersonal difficulties
· Differentiating from axis 1:
o There is substantial comorbidity with axis 1 – but must be distinguished
from axis 1 (which is episodic, different from normal state. Personality
disorders ARE the normal state)
o Need to exclude other possible factors: eg substance abuse, head injury, general medical condition, mood or psychotic disorder (ie must not occur exclusively in the course of an axis 1 disorder)
o Consider axis 2 if: ongoing non-compliance, client unaware of effect of
their behaviour on others, client acknowledges need for change but motivation
is questionable, always blame others for their behaviour
·
Can‟t diagnose before age 19
(much of the description of the disorders is also descriptive of adolescence)
·
Requires longitudinal assessment
and collateral information
·
Must evaluate within a cultural
and religious context (DSM 4 is white & American)
·
Labelling someone with a
personality disorder can be difficult, given limited information and possible
reactions ® often people labelled „traits of disorder X‟
·
Presentation is often not for the
disorder (as it could be, for example, for depression), but for the degree of
impairment due to excessive or little compliance with treatment
·
Treatment is difficult and
long-term: given deeply imbedded nature and genetic predisposition to
personality
· Explanation to client:
o Behaviours were probably adaptive to survive difficult childhood experiences (at some point behaviours were helpful – but they‟ve got stuck). Take care to look for an explanation not someone to blame (people usually do the best they can)
o But it is now more functional to use different strategies in different situations
o Take care of criticising non-compliance: few are proud of „doing what
they‟re told‟ – would you rather be a sheep or an eagle?
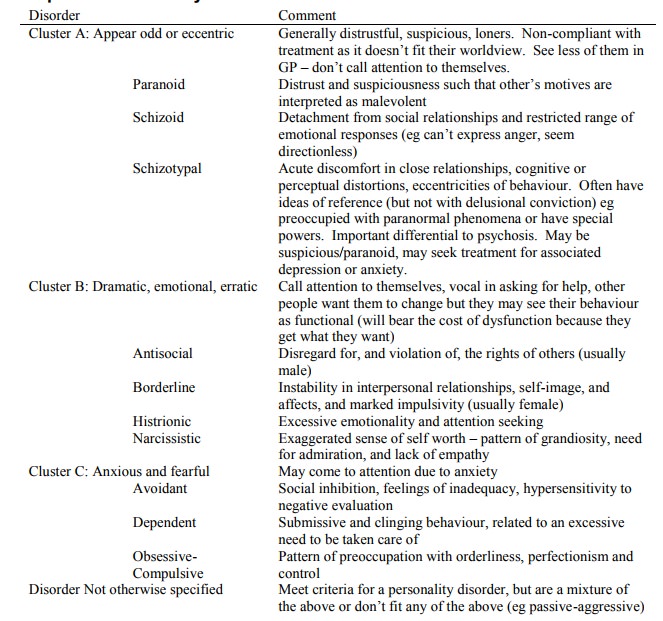
Examples of Personality Disorders
Borderline Personality Disorder
·
Incidence: 3 – 5 % (cf 1% for
Schizoid)
·
Criteria include:
o Frantic efforts to avoid real or imagined abandonment
o Unstable and intense relationships alternating between extremes of idealization and devaluation
o Impulsivity in areas that are potentially self-damaging: eg spending,
sex, substance abuse, binge eating
o Recurrent suicidal behaviour, parasuicides, threats or self-mutilations
o Marked reactivity or mood, difficulty controlling anger
· Characterised by:
o Schema: I can‟t control myself ® overdeveloped emotional responsiveness & underdeveloped self-identity, impulse control
o Core belief about self: I‟m defective, helpless, vulnerable, bad
o Belief about others: other people will abandon me, can‟t be trusted
o Combination of these two leads to extremes of behaviour: need to depend
on others but will be abandoned
o Hate being alone: may attend A & E or ring friends late at night for
company
·
Self-harm:
o Begins between 10 and 16: often following a major life change
o „Toxic self-soothing‟: eases the inner pain – powerful way to feel better. Can either help the dissociation (turn off emotions) or help them feel real
o Communication strategy: there is chaos within family and have never
asked for help ® can‟t ask for help now. But self-harm is not always a cry for help. For
most, self-harm is a private matter
o Strategy in the game of life: to manipulate people or drive them away
o Always need to screen for concurrent depressive episode: this will need
treatment
·
What helps in situations of
self-harm
o Non-judgemental acceptance
o Teach other ways to self-sooth
o Deal with trigger event: what causes the negative feelings
o Address underlying issues: but shouldn‟t do trauma counselling without
also improving coping skills
· Aetiology:
o Genetic loading in temperament: ¯perseverance, impulsivity, ¯affect regulation, stimulation seeking
o Sexual abuse in 75% (but not all severely abused develop the disorder): feeling unsafe, victimisation, trauma, terror
o 75% are female (men more likely to react by becoming antisocial – same motivation but take it out on others rather than themselves – or substance use). Behaviour in collusion with dominant western values (eg emotionality, dependence)
o Other societal factors eg invalidating environments (eg neglect), marginalisation
o Most affected people have this cluster of factors, but someone can still
get it even if the best of upbringings Þ ?stronger than normal
predisposing temperaments
Related Topics