Chapter: Medicine Study Notes : Neuro-sensory
Stroke
Stroke
· = The acute onset of focal or global neurologic deficit presumably of vascular origin lasting > 24 hours (WHO). This includes ischaemic stroke, intracerebral haemorrhage and subarachnoid haemorrhage
· Aetiology:
o Risk in NZ in 65 – 74 is 1:100, in 85+ is 1:30
o 80% due to atheroma, thrombosis and embolism, especially following heart (recent MI, AF, RF disease) or vessel pathology
o Nearly half the people having a new stroke are already in institutional care or needing help with daily activities
o 25% of strokes are in people who have had a previous stroke
· Differential to stroke: TIA, Migraine, Trauma, space occupying lesion (sub-dural haematoma, tumour, abscess), infections, hypoglycaemia, delirium, MS and spinal chord pathology/injury
· Isolated signs seldom due to a TIA or stroke: dizziness, unconsciousness
Site of Lesion
· Site of lesion:
o 75% hemisphere
o 25% posterior circulation
o 20% lacunar
· Pathophysiology: Brain has high and constant need for blood supply
· Signs of cerebral involvement:
o Dominant hemisphere: language disorder (dysphasia, middle cerebral artery)
o Non-dominant hemisphere: disorders of knowing (agnosia) and doing (apraxia), visual or sensory neglect
o Loss of integrated cerebral function (eg cognitive impairment, memory, abstract thought)
· Failure of inhibition of lower centres (eg spasticity and urinary incontinence)
o Seizure activity: abnormal electrical activity in brain tissue around areas of ischaemia
o Hemianopia
o Four classes:
§ Total anterior circulation infarction (TACI. Anterior = Carotid artery Þ anterior and middle cerebral arteries): language or visuospatial disorder (depending on side) + homonymous hemianopia + motor deficit in two or more of face, arm or leg
§ Partial anterior circulation infarction (PACI): 2 of 3 of TACI criteria
§ Posterior circulation infarction (POCI. Posterior = Basilar artery Þ posterior cerebral artery): variety of presentations, including ipsilateral cranial nerve palsy with contralateral motor and/or sensory deficit, isolated cerebellar dysfunction, isolated homonymous visual field defect
· Common lacunar syndromes (small deep white matter infarcts):
o Pure motor hemiparesis
o Pure sensory abnormality
o Ataxic hemiparesis
o Sensori-motor stroke
o Dysarthria and clumsy hand
· Signs of brain stem involvement:
o Diplopia, bilateral weakness or numbness, vertigo, ataxia
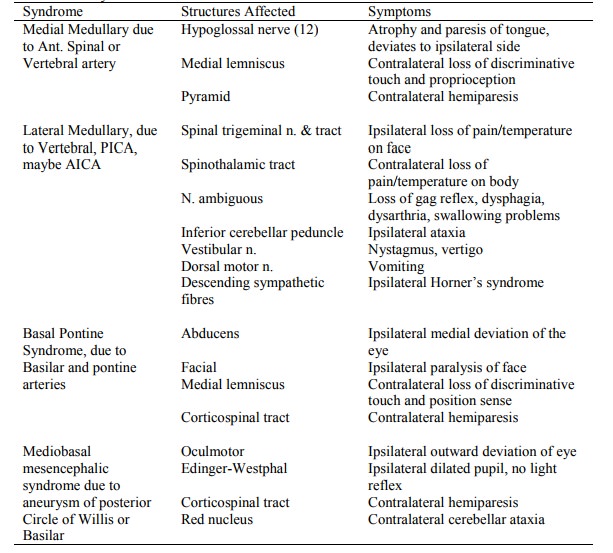
o Brain stem syndromes: *
· Transient Ischaemic Attacks (TIAs):
o 30% of untreated TIAs eventually have a stroke, aspirin reduces this by a quarter
o Presence of carotid bruit not very sensitive for stenosis (ie can have stenosis without it, may not have significant stenosis with it)
o Surgery for carotid stenosis giving TIAs: beneficial if stenosis > 70%, ® ¯risk of ipsilateral stroke. Other studies less variable (NNT if asymptomatic = 17, if symptomatic then 6 – 7)
o Angiogram morbidity = 1.5%, surgical morbidity 1.5 – 6.3% (if not vascular trained)
· Also consider multi-infarct dementia
Management
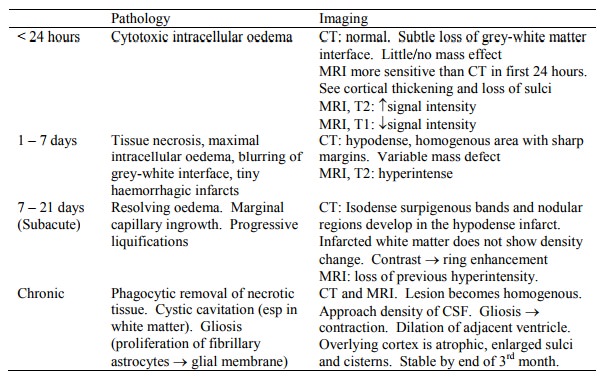
· Investigations:
o FBC: exclude polycythaemia and anaemia. Do electrolytes and renal function
o ESR: exclude vasculitis
o Glucose
o ECG/CXR for heart disease, AF
o ?CT – 5% don‟t have a stroke, also exclude haemorrhage before antithrombotic treatment, and to assess for carotid surgery (>70% stenosis)
· Treatment:
o Aspirin ® small improvement in outcome if not haemorrhagic
o Heparin has a negative effect: although beneficial for DVT prophylaxis
o Warfarin anticoagulation if mitral stenosis or AF
o tPA if within 4 hours and there is visible evidence of infarct covering < 1/3 of MCA territory on CT
o Immediate anti-hypertensive therapy only if hypertensive encephalopathy is suspected (will have papilloedema)
o Assessment of swallowing by a speech-language therapist: 40% of hospitalised stroke patients have swallowing problems, can ® aspiration. Gag reflex is not sufficient to indicate normal swallowing. Nil by mouth until assessed (ie for 12 – 24 hours) unless clearly dehydrated
o Watch for cerebral oedema over next 24 hours if large stroke. Restrict fluids, iv mannitol
o Early rehabilitation: turning to prevent bed sores, limiting bed rest
o Assessment for depression (common following stroke) and urinary incontinence
Prognosis
· After 6 months, 1/3 are dead, 1/3 have moderate disability, 1/3 have good recovery
· Poor prognosis if haven‟t started to make a good recovery after 2 weeks (acute assessment not reliable)
· Risk factors for poor prognosis: prior stroke, persistent incontinence, cognitive/perceptual deficits, poor previous functional status or social supports, poor sitting balance
Vascular Pathology
· Primary intra-cerebral haemorrhage:
o Eg Sub-arachnoid haemorrhage or Intra-cerebral haemorrhage related to trauma
o Due to high blood pressure or lobar haemorrhage (?due to amyloid deposition in vascular walls)
· Ischaemic stroke:
o Thrombotic: occlusion – depending on collateral flow
o Embolic stroke
o Other: vasculitis, cerebral venous thrombosis, carotid artery dissection, etc
· Extent of infarction depends on:
o Adequacy of collateral flow (via circle of Willis). Little/no collateral flow for the deep penetrating vessels supplying the thalamus, basal ganglia, and deep white matter
o Presence of previous occlusive lesions
o Location and rapidity of the occlusive process
· Infarcts are of two types:
o Haemorrhagic (red) infarcts
o Non-haemorrhagic infarcts: pale, bland, anaemic
Thrombotic infarction
· Arterial occlusion usually due to in-situ thrombosis over a plaque, or emboli
· Most common sites for atherosclerotic involvement are:
o Carotid bifurcation
o Origin of the middle cerebral artery
o Either end of the basilar artery
· Healing in the brain: don‟t want scarring as the remaining tissue doesn‟t need protection (it‟s still within the skull) and scar contraction would damage surrounding tracts. So instead of scarring, you get gliosis and cavity formation
Embolic Infarction
· Mural thrombosis ® emboli. Most common sources are plaques within the carotid arteries and cardiac mural thrombi
· Most commonly affects middle cerebral artery
· Embolus responsible for ischaemia lyses within 1 – 5 days ® reperfusion into ischaemic brain (lost the ability to autoregulate)
· This leads to perfusion, especially of grey matter and basal ganglia (lots of capillaries). Oedema (would be ¯ if thrombotic)®mass effect. Cortical petechial haemorrhages. If these are extensive and merge ® haemorrhagic infarct
· CT: previously hypodense become iso/hyper dense
Haemorrhagic Infarcts
· Usually secondary to embolic infarct
· Result from high reperfusion pressure, or following anticoagulation in thrombotic infarcts (eg heparin)
· May develop within 21 days following an embolic infarct
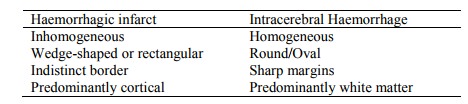
· Difference between haemorrhagic infarct and Intracerebral haemorrhage:
Haemodynamic Infarcts
· ~ Border zone infarcts
· Vaso-occlusive disease + disturbed autoregulation ® temporary uncompensated decrease in perfusion pressure
· Affects watersheds between vascular territories (may ®haemorrhagic infarct), especially between the middle and anterior cerebral arteries
· Can lead to transient ischaemic attacks and infarction
Lacunar Infarcts
· Hypertension ® arteriolar sclerosis of the deep penetrating arteries of the: · Middle cerebral artery ® basal ganglia and internal capsule
· Posterior cerebral and basilar communicating arteries ® mid-brain and thalamus
· Arteriolar sclerosis ® hyaline ® disrupted lumen ® small infarct ® small round lacunae (hole)
Cerebral Venous Occlusion
· Confined to certain patients: pregnancy, post-partum, diabetes mellitus
Related Topics