Chapter: Medicine Study Notes : Neuro-sensory
Focal Ischaemic Retinal Disease
Focal Ischaemic Retinal Disease
·
Affects little vessels
·
Features:
o Cotton wool spots:
§ Fluffy and off-white/yellow
§ Due to micro-infarction ® superficial area of necrosis and oedema
§ Axons are disrupted and become distended (cytoid bodies)
§ Resolve in 6 weeks
o Hard exudates:
§ Discrete, brighter white, often around macula
§ Plasma leaks from damaged capillaries (secondary to thickened basement
membrane) in the outer plexiform layer (deeper in the retina) and forms
proteinaceous lakes
§ Resolves over several months
o Haemorrhage: usually arises from microemboli/thrombi damaging vessels
§ Flame: a small arteriole bursts into nerve fibre layer and spreads along
nerve fibres
§ Dot: capillary bursts into outer plexiform layer
§ Blot: into the subretinal space
§ Roth‟s spots: central white infarct surrounded by haemorrhage
o Microaneurysms:
§ Round or oval dilations of capillaries – look like lots of very little
red dots
§ Central in diabetes, peripheral in central retinal vein occlusion
§ Due to reduced numbers of pericytes surrounding capillaries
o Neovascularisation:
§ Response of the eye to vascular insufficiency, secondary to angiogenesis
factors from ischaemia: proliferate around the margin of non-perfusion. Detect
with fluorescein angiogram
§ Appears as fine lace work of new vessels. They leak and bleed
§ Sites:
·
Iris surface ®
neovascular glaucoma, ectropion uvea
·
Pupillary membrane ®
Posterior Synichiae
o Vitreal Surface ® haemorrhage, pre-retinal fibrovascular membranes ® scarring
® retinal detachment
o Easy to see if over optic disk (normally should only be large vessels)
·
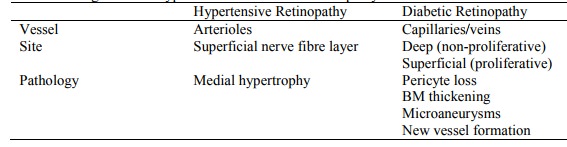
Differentiating between
Hypertensive and diabetic retinopathy:
Diabetic Retinopathy
· Diabetes Mellitus
·
1/3 diabetes with > 30 years
disease will loose some sight. Diabetics 25 times more likely to go blind
·
Risk related to duration Ăž Type 1
(juvenile onset) more likely to cause damage
·
Retinal exam essential:
o At diagnosis for maturity onset (may have had diabetes for 5 – 10 years)
o After 5 years for juvenile onset and annually thereafter
o Fluorescein angiography (injected in arm then photograph retina) to test
for neovascularisation
·
Causes: Thickened basement
membrane of retinal microcirculation ® leakage, oedema, nonperfusion
and micro-aneurysms
·
Macular retinopathy: boggy, leaky
macula ® blurred vision
·
Non-proliferative retinopathy (= Background Retinopathy): Progression:
oedema (® blurred vision) ®
microaneurysms ® hard exudates ® cotton wool spots ® small haemorrhages ® venous bleeding
·
Proliferative retinopathy:
o Neovascularisation
o Retinal detachment due to shrinkage of subsequent scars
o Vitreous haemorrhage (can also be due to vitreous collapse tearing at
retina or retinal venous occlusion – usually due to ÂBP ® expanded
artery ® compresses adjacent vein)
·
Treatment:
o Regular checks
o Blood sugar control
o Treatment of vascular disease (eg ÂŻBP)
o Laser treatment (photocoagulation): 2 – 3,000 burns (but NEVER on
macula). ÂŻO2
demand ®
o ÂŻneovascularisation. Complications: ÂŻperipheral
and night vision, macula oedema
o Vitrectomy: if non-resolving vitreous haemorrhage or fibrovascular
contraction of vitreous (which has risk of ® retraction of retina ® tear)
o Retinal repair: reattach retina
·
Diabetes can also cause:
neovascular glaucoma (blocking flow past lens), more susceptible to damage from
ÂIOP, cataract, extraocular muscle palsy
Hypertensive Retinopathy
·
Rarely causes visual loss. Requires diastolic BP > 120 for many years
·
Stages:
o Stage 0: no changes
o Stage 1: „copper-wiring‟ of arterioles due to thickening of the walls
due to medial thickening (very subjective)
o Stage 2: Arteriovenous nipping –
thickened arterioles compressing underlying veins
o Stage 3: Soft-exudates and/or flame haemorrhages (spread longitudinally
along fibres)
o Stage 4: Papilloedema plus the above
·
Bilateral and symmetric. More cotton wool spots (nerve fibre hypoxia)
·
Retinopathy regresses if
hypertension controlled (cf diabetes which doesn‟t)
Related Topics