Chapter: Medicine Study Notes : Neuro-sensory
Physical Exam - Neurology
Physical Exam
·
Hard to incorporate with rest of
physical exam Ăž do it on its own
· Tailor the exam to the clinical problem (full exam can take an hour)
·
Avoid suggestion: rather than „Is
this sharp‟ or „do you smell the perfume‟ say „what do you feel/smell‟
·
Quick list:
o Observe: including wasting and fasciliculations
o Cranial nerves
o Tone
o Power
o Reflexes
o Coordination
o Sensation: position, vibration, pin prick, light touch
Mental State Exam
·
Wanting to test:
o Distributed cognitive function:
§ Attention/concentration
§ Memory
§ Word finding
o Localised cognitive functions
§ Speech
§ Visuo-spatial
·
If suspicious from history need
assessment of the following:
o State of consciousness: alert, drowsy, stuporose, comatose (assess with
GCS)
o Other observations from mental state exam
o Orientation: date, their name, age, who are their relatives
o Remote or long-term memory: phone number, Prime Minister, recent events
in the news
o Registration and Immediate recall: Memorise 3 objects, recall after 3
minutes. Repeat 4 or 5 digits in reverse
o Others: abstract thinking, serial 7‟s
·
Can use Mini-mental status test:
but not sensitive to subtle impairments
Language
·
If difficulty following
instructions, appears confused, etc
·
Requires assessment of spoken and
written response to both spoken and written questions
·
Observations: fluency, word
finding, grammatical errors, understanding questions
·
Naming objects: ask about whole
object then parts – wrist watch and strap
·
Repetition: No Ifs ands or buts
·
Auditory comprehension:
Increasingly complex commands, eg Close your eyes, touch your left ear with
your right thumb and stick out your tongue
·
Writing: write a simple sentence,
their name and address
·
Reading: read aloud
Cranial Nerve Exam
·
1: Olfactory: Smell. Not if doing general screen. Close eyes. Check each
nostril patent then test (eg scented soap on ward). Poor smell common (smoking,
allergies, ageing). Also in Alzheimer‟s, Parkinson‟s, MS, chemotherapy. Most
serious association: frontal lobe tumour, presents with personality change,
self-neglect, dementia
·
2: Ophthalmic nerve: lesions common and serious. Check if they normally wear glasses. Test:
o Acuity: (use pinhole if they‟ve forgotten their glasses). Test each eye separately
o Visual fields: confrontational testing: first just hold hands in each
visual field and ask what they see. Then wiggle one finger, then the other,
then both, in all visual fields (or count fingers)
o Red pinhead test: test for colour sensitivity – more sensitive than
acuity (good for vague hemianopia). Loss of colour = “desaturation”. Blind spot
= “scotoma”
o Hemianopia:
§ Pituitary lesion ® bitemporal hemianopia (nasal retina affected). Bring red pin from affected field into normal – gain of red colour is convincing. Upper temporal field in one eye is typically affected first
§ Parietal lesion ® visual inattention
·
3, 4, 6: Seeing double. Complicated to sort out
o Look for ptosis
o Smooth tracking: Fix on finger, draw H in the air, ask for report of
diplopia, watch for one eye lagging or nystagmus (a few beats in extreme gaze
is normal)
o Examine pupils at rest, light reflexes and near reflex
o Voluntary eye movement:
§ Look up, down, left, right. Often
elderly have trouble looking up anyway
§ Cover test: look at target, cover one eye, does other eye move? Reverse.
Shows which is fixing eye
§ If diplopia found, find field where it‟s maximal. Weak eye moves less; good eye overshoots.
§ Use stick man drawn on tongue depressor
§ Problems locating target (overshoot and come back) ®
?cerebellar
·
5: Trigeminal Nerve
o Sensory 5th: Test light touch and pinprick in all 3 divisions on both sides
(separate pathways in the brain stem). Test corneal reflex (early sign of
lesion) – patient looks up, use cotton wool on cornea (more sensitive than
sclera)
o Motor 5th: jaw opening in midline (tests pterygoids). Jaw deviates to the side of
weakness. Clench jaw and palpate maesseters. Jaw jerk only if indicated
·
7: Facial Nerve. Wrinkle forehead
and „show your teeth‟ (not smile). Look for lower face weakness. Upper face (eg
screw up eyes) better preserved in UMN, both similarly affected in LMN (eg
Bell‟s palsy – can be due to HSV, onset in days, recovery in weeks/months,
rarely parotid tumour). Note symmetry, fasciculation, and abnormal movements.
Don‟t normally test taste
·
8: whispered voice at arms
length, with patient‟s eyes close. Mask opposite ear by rubbing your finger and
thumb together beside it.
·
9 (glossopharyngeal and vagus
nerves): back of mouth, say ahh, uvula up in midline. Check swallowing. Gag
normally not tested – if you do, test both sides. Unilateral absence abnormal,
bilateral absence may be normal.
·
11 (accessory): shake and shrug
shoulders. Observe sternomastoid and trapezius at rest for wasting,
fasciculation, or dystonia. Look sideways, try to return head against
resistance. Compare strength of shoulder shrug on each side. Rarely useful,
unless confirming site or suspected lesion. Always test neck extension if
diffuse muscle weakness – if abnormal indicates lesion above C1/C2
·
12: Hypoglossal nerve. Tongue.
Examine at rest then protrude. If fasciculation ® ?motor
neuron disease. Deviates towards the weak side. Push tongue into check against
your finger. Try rapidly alternating movements of protruded tongue or rapid
la-la-la
Motor Examination
·
Observation for congenital maldevelopment,
wasting, fasciculation and abnormal movements (tremor, chorea, myoclonus, dystonia)
·
Assessment of tone: resistance to passive movement
(must be relaxed). ÂTone due
to:
o Rigidity (Basal ganglia): uniform resistance to slow passive movement,
may be jerky (cogwheel rigidity). Affects flexors and extensors equally
o Spasticity (upper motor neuron). Rapid passive movement ® maximal
tone to start with, decreases suddenly as muscle is lengthened. Most marked in
flexors of arms and extensors in legs. Due to reflex contraction to muscle
stretch
o Clonus: maintaining stretch (eg of ankle plantar flexors) ® further
repetitive beating
·
Power:
compare between sides
o Test in position where patient has mechanical advantage: you shouldn‟t
be able to win then if its normal
o Grade as follows:
§ 0: no contraction
§ 1: a flicker/trace of contraction
§ 2: active movement with gravity eliminated
§ 3: active movement against gravity but not against resistance
§ 4: active movement against gravity and resistance, but reduced power
(covers wide range – can classify as mild, moderate or severe weakness)
§ 5: normal power
·
Motor exam of the arms:
o Observe arms at rest, then outstretched with eyes closed (check for
drift – non-specific test). Look for wasting of 1st dorsal interosseus and abductor
pollicis brevis
o Assess tone at elbow (flexion/extension and supination) and wrist
(flexion/extension) with slow and rapid movements
o Arms (start at top and work down)
§ Shoulder abduction (deltoid, C5, axillary nerve). Arms out like chicken wings – push it down
§ Elbow flexion (biceps, brachialis, C5-6, musculocutaneous nerve) – pull me in
§ Elbow extension (triceps, C7, radial).
Arm bent up in front - push me out
§ Wrist extension. (Extensor carpi ulnaris and radialis, C6-7, radial
nerve). Extended „cocked‟ wrist – push it down
§ Finger extension (extensor digitorum, C7). Fingers straight out – push
them down just distal to MP joint
§ Finger flexion (flexor digitorum, C8).
Try to uncurl curled up fingers
§ Abduction of index finger (ulnar nerve, T1, dorsal interosseus)
§ Abduction of thumb (median nerve, T1, abductor pollicis). Try and push
raised thumb down into palm. Look for atrophy of thenar eminence
·
Motor Exam of the legs:
o Observation of legs: while standing, walking, lying down. ALWAYS observe
posture and gait: movement of arms, stride length, broadness, smoothness. Stand
with eye‟s closed and feet together (Romberg test). Look for wasting of
tibialis anterior and small muscles of feet
o Check for tone
o Check for clonus. Flex hip and knee to 45 degrees, externally rotate
hip, rapidly dorsiflex foot and hold. Two or three beats of clonus may be
normal if symmetrical
o Power in Legs (patient lying down):
§ Hip flexion (ilio-psoas, L1-2, lumbar plexus). Push down on raised straight leg
§ Hip extension (gluteus maximus, sciatic nerve, L5-S1). Lift ankle of
straight leg
§ Knee Extension (quadriceps, femoral n, L3-4). Bend knee, try to push ankle in
§ Knee Flexion (hamstrings, sciatic nerve, L5 – S1)
§ Ankle dorsiflexion (tibialis ant peroneal n, L4 – 5): push on top of
foot while toes raised
§ Ankle plantarflexion (gastrocnemius, sciatic nerve, S1 – 2): push on
bottom of foot
§ Ankle inversion (tibialis ant & Post, peroneal and tibial n, L4 – 5).
Patient bends foot in and try and pull it back
§ Ankle eversion (peronei, peroneal nerve, L5 – S1): Patient bends foot
out and try and pull it back
o Rapid leg tests:
§ If they can walk on their heals, then no foot drop (L5 or common
peroneal)
o If they can walk on their tiptoes, then no S1 lesion (plantar-flexion)
o To test proximal leg function, crouch and stand up
·
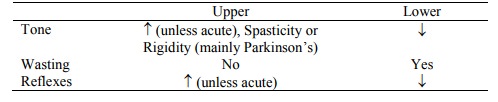
Differentiating Upper and Lower
Motor Neuron lesions
Reflexes
·
Key is for them to be relaxed
·
Arm (Clench teeth if no
response):
o Biceps (C5/C6)
o Triceps (C7)
o Supinator (C5/C6)
o Can also do finger reflex if suspect C8 lesion: tap your fingers while
placed over outstretch fingers of face up hand. Often normally absent
·
Leg (if no response, interlock
fingers of both hands and pull just before tap)
o Patella (hold knees up) (L3/L4)
o Ankle (passively dorsiflex ankle) (S1). 3 ways: hand on dorsum of foot
and tap hand, directly on Achilles tendon, or kneel on chair with foot hanging
off, tap Achilles tendon (most sensitive)
·
Grading reflexes:
o 0: absent
o +-: just present
o +: normal
o ++: brisk normal
o +++: very brisk
·
Plantar responses: put patient at
ease! Normal response is plantar flexion (down). If upper motor neuron lesion,
big toe up and other toes fan out (Babinski). Not positive if withdrawal
response (hip and knee flexion) due to over response
·
Superficial Abdominal reflexes:
Not tested routinely. Stroke lightly with sharp object in each quadrant towards
midline. Normal reflex is contraction. Tires quickly
Co-ordination
·
Rapid alternating movements of
hand: supinate and pronate hand rapidly (dysdiadokinesia)
·
Finger-nose-finger test. Not too fast (may mask intention tremour)
·
Heel-knee-shin test
·
Heel-toe walking: tests midline
cerebellar vermis
·
Romberg: tests dorsal column sensory
loss (ie proprioception). Rare in
clinical practice
·
Important syndromes including
ataxia:
o Cerebellar haematoma: Sudden onset of progressive headache, vomiting,
and inability to stand or walk. Later progressive drowsiness, lateral gaze
palsy from pontine compression. Decompressive surgery can be lifesaving
o Wernicke‟s Encephalopathy: Confusion, ataxia, nystagmus. 6th nerve palsy. On recovery:
impaired short-term memory, confabulation. Common with prolonged vomiting, poor
nutrition, not confined to alcohol
Sensory test
·
Issue is where and why to test.
What do you expect to find? Do this last so you have some idea what to look
for. Very easy to suggest to patient
·
Common scenarios:
o Hemisensory loss: stroke, peripheral root and nerve lesion
o Glove or stocking: spinal chord lesion or peripheral neuropathy
·
Get patient to close eyes.
Stimulate at irregular intervals so patient can‟t anticipate them. Test from
abnormal to normal. Don‟t try to completely map – just test key boundaries
·
Key Dermatomes:
o Stand on S1
o Sit on S3
o Groin: L1
o Umbilicus: T10
o Nipple: T5
o T2 meets C4 on line connecting axilla: should be clear difference across
this line in any lesion between T2 and C4
o Middle Finger: C7
·
Position sense: hold big toe by the sides, explain
which way is up and down, then test. Has
low yield in practice. Try functional test: can they stand up with eyes closed?
·
Vibration: 128 Hz fork. On bony
prominences (what do you feel?). Move up until its positive. Bunion ® medial
melleolus ® tibial tuberosity ® anterior iliac spine. Test fingers for completeness. First sensation to
go in progressive deterioration
·
Pinprick: Use large safety pin
and discard after use. Toes, fingers, face (no more unless suspicious, eg ÂŻ reflexes).
Is it sharp or blunt? Can alternate sharp and blunt end to see if they can tell
the difference. More reliable than light touch if both damaged
·
Temperature: Not usually done if
pin prick done
·
Light touch (cotton wool)
·
Others (not routine):
o Two point discrimination
o Stereognosis: recognising objects by their feel (coin, key, etc). Normal hand first
o Graphaesthesia: write numbers on the hand
o Sensory inattention: touch sides separately and together – which is
being touched?
Related Topics