Chapter: Medicine Study Notes : Neuro-sensory
Epilepsy
Epilepsy
·
Epilepsy in Childhood, Benign Febrile Convulsions and Anoxic Seizures
· 1:200
·
Onset after age 20 Þ 10%
chance of tumour
·
Symptoms:
o Abrupt onset, brief duration, rapid recovery, and stereotypical
recurrence
o Not just fits: focal signs depending on where in the brain it arises
·
Very long list of differentials
to epileptic seizure: See Other Spells,
·
Is it epileptiform:
o Pseudo-seizure (or Non-Epileptic Seizure): either factitious disorder (are deliberately faking) or conversion disorder (they think it‟s real)
o Hard to differentiate: going blue, frothing at mouth and incontinence
can happen in pseudo-seizure. Epiletics may not have post-ictal phase
o Gold standard is EEG: but can‟t do this in A&E. Fall back is
checking whether the person is in any way aware (then it can‟t be generalised)
– eg localising to pain (sternal rub, squeeze thumb nail), drop their hand onto
their face
o Check history: evidence of brain injury, infection, on anticonvulsant
meds
o Pseudo seizure more common in women (10:1) and those with a medical
connection (eg doctor/nurse in family, someone with epilepsy)
·
Epileptic seizures happen more
if: tired, ill, fever, stressed, not taking medication (but these are not
classified as „provoked‟ as they wouldn‟t provoke a seizure in a normal person)
Seizure Types
·
Generalised: bilaterally
symmetrical without local onset
o Tonic-clonic (Grand mal) seizures: Tonic phase: 10 – 20 secs – extension phase then tremour
o begins – repetitive relaxation of tonic contraction. Clonic phase: usually 30 seconds, random movements, tongue often bitten
o Absence (Petit Mal) Seizures: Characteristic type of absence attack. Childhood or adolescent onset, associated with 3/sec spike and wave on the EEG. Blank stare and unresponsive for 5 – 15 seconds. No post-ictal confusion or sleepiness. May also have automatisms and mild clonic motion (usually eyelids at 3 Hz). May be induced by hyperventilation. 80% have no further seizures after 20 years old. Can also have atypical absence seizures. Treat with ethosuximide or sodium valproate
o Atonic: complete, sudden loss of tone – completely collapse, may injure
themselves
o Tonic: sustained contraction, maybe with fine tremour
o Myoclonic: Sudden, very brief jerk but still generalised
o Clonic: rhythmic jerking
o Infantile spasms:
§ Sudden bilateral symmetrical jerk, extensor or flexor. Can be subtle, come in clusters
§ Usually around 3 – 6 months, boys > girls
§ Grow out of the spasms
§ Bad prognosis: cerebral palsy, retardation, etc
§ Medical emergency: try to urgently get them under control
·
Partial: Begin locally
o In simple partial seizures consciousness is preserved.
o Complex partial seizures are focal seizures in which consciousness is altered (eg blank unresponsiveness followed by automatisms, eg lip smacking, other semipurposeful activity) – usually temporal lobe but may be frontal. Can go on for minutes. Aware it is coming (cf absence which is sudden)
o Partial seizure secondarily generalised: they have an awareness first
o Localising it:
§ Preceding aura: olfactory, visceral, auditory, visual, déjà vu
§ Dystonic posturing: contraction of agonist and antagonist muscles
§ Post-ictal Todd‟s Syndrome: if they have one area of weakness after a
seizures (ie one hand weaker than the other) then it started locally
·
Automatic behaviour usually seen
in complex partial seizures: but can be in absence (petit mal) seizures. Eg
Oral or manual automatisms
· Seizure location:
o Frontal: focal tonic or clonic motor activity, posturing, prominent
motor automatisms but no orofacial or experiential automatisms
o Central: focal clonic seizures with preservation of awareness
o Temporal: experiential, gustatory or olfactory hallucination. Motion arrest, automatisms
o Parietal: exclusively somatosensory manifestations
o Posterior: polymodal sensory, visual, auditory or somatosensory
hallucinations
·
Sorting out type of seizure:
o When do the seizures occur
o Does patient know they‟re going to have a seizure
·
What can the patient recall
·
Detailed description from
observers:
o Are they aware – will they respond
o Are their automatisms
o Is there dystonic posturing
o How long did it last
·
After the seizure: are they
confused, can they speak, any post-ictal Todd‟s
Treatment
·
Diagnosis is clinical. EEG helps
with severity, classification, to localise a surgically remediable abnormality
(eg hippocampal sclerosis), and to differentiate pseudo-seizures
·
Don‟t treat until you‟re sure it‟s
epilepsy
·
Anticonvulsants suppress seizure
activity in 80%
· Principles of drug treatment:
o When to treat: often wait for second seizure – although treatment after the first ® ¯occurrence, but no long term change in outcome
o Use only one drug
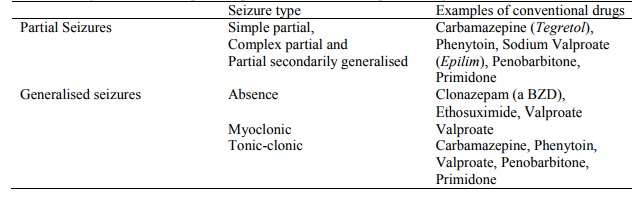
o Tailor drug to seizure type
o Introduce slowly. Takes about 5 days to stabilise a change in dose
o Monitor drug level: for other than phenytoin, this is to check
compliance. Beware – plasma level at which seizure control is obtained is
variable
o Consider withdrawal of drugs after 2 years without seizure, slowly over
6 months
·
Mode of action unknown – but may ¯GABA
breakdown, as well as modifying flux of Na, K and Ca ions
·
Usual drugs:
o Idiot‟s guide: carbamazepine for partial seizures and Valproate for
generalised
·
Conventional drugs have hepatic
clearance
· Side Effects:
o General lethargy, ¯concentration, unsteadiness, dizziness
o LFTs: but
serious hepatotoxicity rare. Especially
Valproate
o Rarely bone marrow suppression
o Pregnancy:
§ Epilepsy often worsens during pregnancy
§ Plasma concentration of drugs falls due to pharmokinetic changes and ¯compliance
§ Teratogenic: 3% risk of malformation on 1 drug (also, epilepsy itself can be teratogenic - ?hypoxia during seizure)
§ % in breast milk varies by drug
o Specific drugs:
§ Carbamazepine: enzyme inducer
§ Phenytoin: Dose-dependent kinetics ® small in dose
may ® in plasma concentration,
§ SE: ataxia, peripheral neuropathy, gingivitis
·
Must be seizure free (with or
without treatment) for 12 months before you can drive. Obliged to tell
·
LTSA on diagnosis if the patient
won‟t and continues to drive
Status Epilepticus
·
Repeated seizures without
regaining consciousness
·
No one knows how long is too
long: but after 10 minutes risk of damage
·
If not sure whether it‟s
epileptiform then must still treat for status
·
Treatment:
o Protect and maintain airway, insert oral airway
o Prevent injury
o 100% oxygen
o Diazepam 10 – 20 mgs iv, not exceeding 2 – 5 mgs per minute. If no iv
access give rectally with 10 – 20 ml normal saline. Duration is brief and
another anticonvulsant is required. Avoid repeating diazepam ® cardiorespiratory
collapse. If no response give clonazepam 1 – 4 mg iv
o Phenytoin 50 mg/min iv (25 mg/min in cardiovascular disease), usual
adult dose 1250 mg in 100 mls saline over no more than 20 minutes. Monitor BP
and heart rate
o If established, give phenobarbitone
o If refractory, then anaesthesia with propofol or thiopentone. Taper after 12 – 24 hours
Other Spells
·
Commonly misdiagnosed as seizures
·
Paroxysmal non-epileptic events
without altered consciousness: Jitteriness, migraine with focal aura, hyperventilation,
acute paroxysmal vertigo, shuddering attacks, anxiety states (eg panic attack),
psychosis, drug induced dystonias, masturbation, tics, etc
·
Paroxysmal non-epileptic events
with altered consciousness: Day dreaming, breath holding spells, reflex syncope,
TIAs, psychosis, pseudo-seizures, delirium, metabolic disorders, other brain
insult (infection, haemorrhage), ritualistic movements, migraine, arrhythmias,
drugs substance abuse
·
Paroxysmal non-epileptic events
related to sleep: benign sleep myoclonus of infancy, head banging, night
terrors, hypnogogic jerks, sleep walking, sleep apnoea
Related Topics