Chapter: Pharmaceutical Biotechnology: Fundamentals and Applications : Formulation of Biotech Products, Including Biopharmaceutical Considerations
Potential Pitfalls in Tumor Targeting
Potential Pitfalls in Tumor Targeting
Upon IV injection, only a small fraction of the homing
device–carrier–drug complex is sequestered at the target site. Apart from the
compartmentalization of the body (see above: anatomical and physiological
hurdles) and consequently the carrier-dependent barriers that result, several
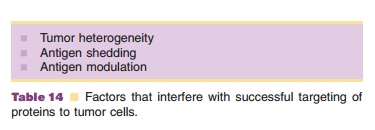
other factors account for this lack of target site accumulation (Table 14).
How successful are MAb in discriminating target cells (tumor cells) from
non-target cells? Do all tumor cells expose the tumor-associated antigen? These
questions are still difficult to answer (Hellstro¨m et al., 1987). Tumor
cell-surface specific molecules used for homing purposes are often
differentiation antigens on the tumor cell wall. These structures are not
unique since they occur in a lower density level on non-target cells as well.
Therefore, the target site specificity of MAb raised against these structures
is more quantitative than qualitative in nature.
Another category of tumor-associated antigens are the clone-specific
antigens. They are unique for the clone forming the tumor. However, the
practical problem when focusing on clone-specific antibodies for drug targeting
is that each patient probably needs a tailor-made MAb.
The surface “make-up” of tumor cells in a tumor or a metastasis is not
constant; neither in time nor between cells in the same tumor. There are many
subpopulations of tumor cells and they express different surface molecules.
This heterogeneity means that not all cells in the tumor will interact with
one, single targeted conjugate. Antigen shedding and antigen modulation are two
other ways tumor cells can avoid recognition. Shedding of antigens means that
antigens are released from the surface. They can then interact with circulating
conjugates outside the target area, form an antigen–antibody complex and neutralize
the homing potential of the conjugates before the target area has been reached.
Finally, antigen modulation can occur upon binding of MAb to the cell surface
antigen. Modulation is the phenomenon that upon endocytosis of the (originally
exposed) surface antigen–immunoconjugate complex, some of these antigens are
not exposed anymore on the surface; there is no replenishment of endocytosed
surface antigens.
Four strategies can be implemented to solve problems related to tumor
cell heterogeneity, shed-ding and modulation. (i)
Cocktails of different MAb attached to the toxin can be used. (ii) Another approach is to give up striving for complete target cell
specificity and to induce so-called “bystander” effects. Then, the targeted
system is designed in such a way that the active part is released from the
conjugate after reaching a target cell, but before the antigen-conjugate
complex has been taken up (is endocytosed) by the target cell. (iii) Not all surface antigens show shedding or modulation. If these phenomena
occur, other antigen/MAb combinations should be selected that do not
demonstrate these effects. (iv) At the present, injection of
free MAb prior to injection of the immunoconjugate is under inves-tigation to
neutralize “free” circulating antigen; then, the subsequently injected
conjugate should not encounter shedded, free antigen.
In conclusion, targeted (modified) MAb and MAb-conjugates are now
studied to assess their value in fighting life-threatening diseases such as
cancer. During the last decade, technology has evolved quickly; many different
new options became avail-able. Lack of detailed pathophysiological and cell
biological knowledge about the behavior of tumors, for instance, slows down
progress. It is even possible that the whole concept of MAb-(conjugates) will
turn out to be only of limited therapeutic value, because ofproblems such as
tumor cell heterogeneity, poor access to tumors and immunogenicity concerns.
Related Topics