Chapter: Biology of Disease: Disorders of the Immune System
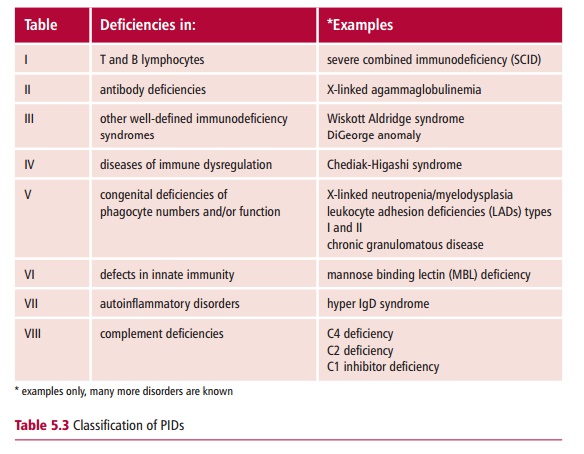
Phagocytic defects - Primary Immunodeficiency Disease
Phagocytic defects
Phagocytic cells, such as monocytes, macrophages and
neutrophils, form part of the nonspecific immune defense. These cells kill
ingested bacteria using several different mechanisms as described. A defect in
any of these mechanisms can lead to increased incidences of infections. Thus,
patients may be severely compromized by defective phagocytes, even if their B
and T cell populations and functions are normal. Some examples of phagocytic
defects are chronic granulomatous disease and leukocyte adhesion deficiency.
Chronic granulomatous disease (CGD) is named from the
granulomatous inflammatory nodules that present on the skin and in the
gastrointestinal and genitourinary tracts. It is an inherited disorder of
phagocytic cells characterized by their inability to generate the reactive
oxygen intermediates needed to produce bactericidal compounds, such as hydrogen
peroxide. The formation of reactive oxygen intermediates is dependent on NADPH
oxidase activity. This enzyme is composed of four subunits and a defect in any
one of them can result in CGD. Approximately 65% of all CGD cases is due to a
defect in the CYBB gene located on
the X chromosome which encodes cytochrome b245.
The genes for the other subunits are located on autosomal chromosomes and
females and males are equally affected. The incidence of CGD is estimated to be
about one in 200 000 to 250 000.
Sufferers of CGD usually present before the age of five years.
Skin infections, pneumonia, gastroenteritis, perianal abscesses are common.
Abscesses on internal organs, such as the lungs, spleen and liver, may also be
present. The small amounts of hydrogen peroxide produced by CGD patients makes
them resistant to catalase negative bacteria. However, catalase positive
bacteria, by definition produce catalase, which catalyzes the degradation of
hydrogen peroxide; hence these types of bacteria give rise to infections in CGD
sufferers. Pneumonia is generally associated with fungal infections; and
disseminated fungal disease also occurs.
A diagnosis of CGD takes into account the recurrent infections
of early onset, granulomas, hepatosplenomegaly, that is enlarged liver and
spleen, and lymphadenopathy. Laboratory investigations include the nitroblue
tetrazolium (NBT) test to determine the activity of the NADPH oxidase. In
neutrophils with normal levels of enzyme, the pale yellow NBT is reduced to a
blue colored compound as NADPH is oxidized, and can be observed in the
cytoplasm. Patients with CGD are treated with high doses of antibiotics over
long periods of time. This treatment also helps to dispel the granulomas.
Abscesses may need to be drained. Bone marrow transplantation has been used
successfully to treat some patients.
Leukocyte adhesion deficiency (LAD) occurs in two forms, but
both are caused by the failure of leukocytes to express cell adhesion molecules
essential for their movement through blood vessel walls during inflammation.
Thus phagocytes are unable to enter inflamed tissues and remove bacteria. In
LAD I, patients do not express the integrin, CD18 on neutrophils, macrophages
and lymphocytes that allows them to bind to endothelial cells lining the blood
vessels. In addition, CD18 is the receptor for C3b, which is an opsonin for
phagocytic cells and crucial molecule of the complement pathway. Patients
suffer localized bacterial infections that may become life threatening. In LAD
II leukocytes fail to express ligands for other cell adhesion molecules, namely
E and P selectins. Binding of leukocytes to these ligands allows them to roll
along the endothelial cell surfaces before crossing into the tissues. Both LAD
I and LAD II are autosomal recessive disorders. While LAD I affects all ethnic
groups, LAD II has only been reported in people of Middle Eastern origin.
Patients with LAD I suffer localized bacterial infections that
may become life threatening. Children do not usually survive beyond two years
of age unless they have a bone marrow transplant. Patients with LAD II also
suffer repeated infections as well as severe growth and mental retardations.
Blood counts from patients with either form of LAD show a leukocytosis, that
is, a white blood cell count in excess of 20 q 109 dm–3 in the absence of infection,
compared to normal values of 4–11 q 109 dm–3 . Both diseases may be diagnosed
by flow cytometry, to assess the presence of the cell adhesion molecule on
blood leukocytes. Leukocyte adhesion deficiency I has been treated successfully
with bone marrow transplantation .
Related Topics