Chapter: Biology of Disease: Disorders of the Immune System
Immunological Hypersensitivity
IMMUNOLOGICAL HYPERSENSITIVITY
Immunological hypersensitivities are disorders in which the immune response to a foreign immunogen results in tissue damage. The term allergy, which originally meant ‘altered reactivity’, is sometimes used synonymously with hypersensitivity. In fact, allergies are only some specific types of hypersensitivity. Although the wordhypersensitivity implies an overreaction, in fact, there is nothing essentially abnormal about the immune response in these cases. It may simply be the extent and nature of the exposure to the immunogen that results in the damage. Indeed, immunogens that provoke hypersensitivities are often ‘harmless’ in that they are not necessarily infectious agents. Immunological hypersensitivities represent the most common group of immunological disorders and, collectively, affect approximately 10% of the population.
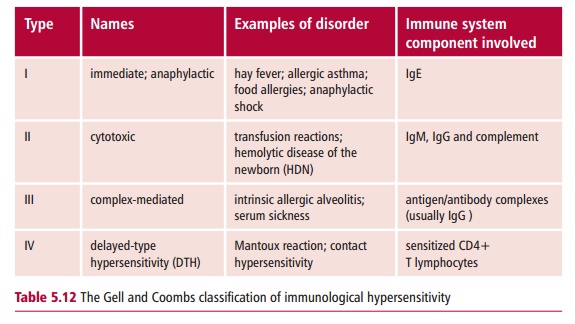
In 1963, Gell and Coombs classified hypersensitivities into four ‘types’ based on the part of the immune system that caused the tissue damage (Table 5.12). This classification scheme is still used today, although not all hypersensitivities belong exclusively to one type. For example, immunological reactions to drugs can be both Types I and III, while intrinsic allergic alveolitis has components of Types III and IV. In addition, expansion of the classification to include further types has been suggested.
TYPE I HYPERSENSITIVITY
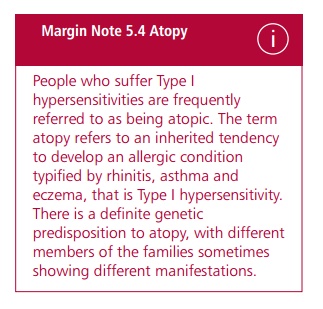
Type I hypersensitivity is also referred to as immediate, because its effects are apparent within eight h of exposure to an immunogen. The effects can be fairly trivial, as in hay fever, or life threatening, as in atopic (Margin Note 5.4) or allergic asthma or anaphylactic shock. The term allergy is often used for Type I, although this is also used for some of the other types. Immunogens that cause allergies are often referred to as allergens and this is the term that will be used here.
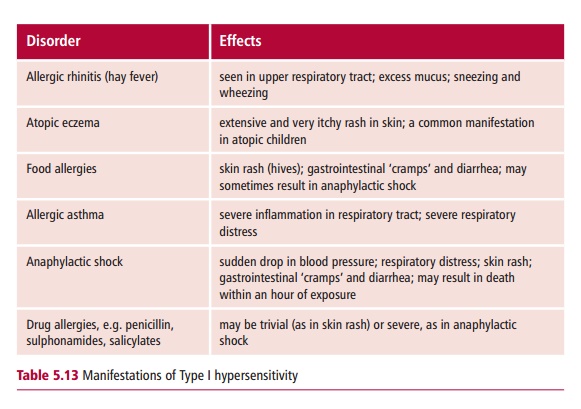
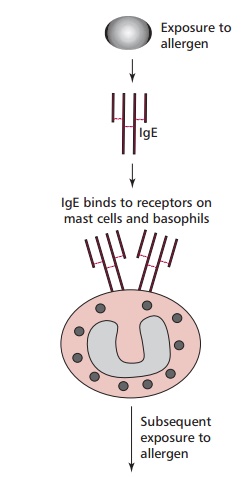
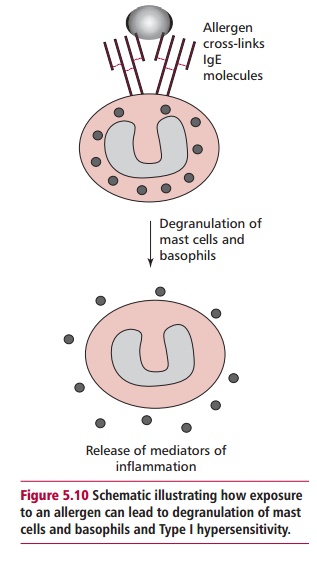
The different manifestations (Table 5.13) of Type I depend on the degree of previous exposure to the allergen and also on the route of exposure. The underlying cause is the production of IgE in response to an allergen. This type of antibody stimulates inflammatory responses that are aimed at eliminating parasitic worms. Atopic individuals produce IgE in response to allergens that, in nonallergic individuals, would stimulate the production of IgG. The tissue mast cells and blood basophils have receptors for the Fc region of IgE, so that IgE binds to the surface of these cells. The more sensitized an individual, the more their mast cells are coated with IgE. Further exposure to the same allergen results in the cross-linking of mast-cell bound IgE by the allergen (Figure 5.10). This triggers an explosive degranulation of the mast cell that releases pharmacologically active mediators, including histamine, which causes vasodilation, smooth muscle contraction and mucus secretion, depending on where they are released. In addition the subsequent release of further mediators, for example leukotrienes and prostaglandins, which are synthesized at the mast cell membrane potentiate inflammation and smooth muscle contraction. This response which evolved as a defense against multicellular parasites, causes the characteristic symptoms of the hypersensitivity.
Type I hypersensitivity is the most common form of the immunological hypersensitivities and is estimated to affect between one in 5–10 individuals, with conditions, such as allergic rhinitis, allergic asthma and food allergies.
Allergic rhinitis
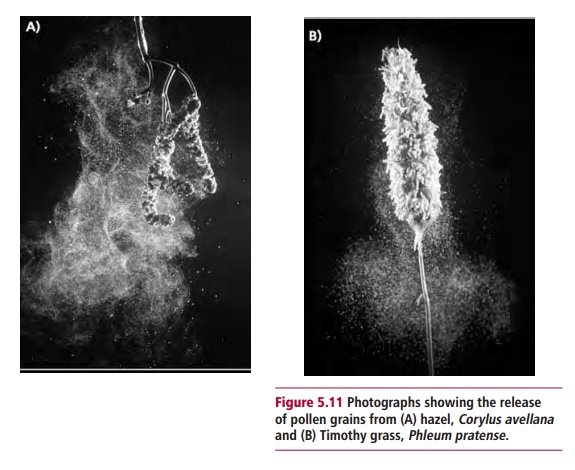
Allergic rhinitis or hay fever is extremely common and its effects are well known. Seasonal allergic rhinitis typically presents in the spring and summer and is generally brought on by pollen to which the individual has been sensitized. Some individuals show sensitivity to many types of pollen (Figure 5.11), including well-known ‘culprits’ such as ragweed, while others are allergic to a single type of tree pollen. Individuals who suffer allergic rhinitis all year round are most likely to be allergic to other types of allergens, such as the dead skin cells sloughed from household pets, or the feces of house dust mites (Figure5.12)which thrive in warm, carpeted dwellings. Although allergic rhinitis isnot life threatening, it can be very debilitating.
Allergic asthma
Allergic asthma is a serious and potentially life-threatening condition brought on by air-borne allergens, such as those which trigger hay fever. In patients with allergic asthma, sensitization to a range of air-borne allergens stimulates inflammation in the respiratory tract, narrowing the airways and eventually leading to hyperreactivity of the muscles of the bronchial tree. The condition is very distressing particularly during an asthmatic attack, when severe respiratory distress may require emergency treatment. The incidence of asthma is increasing in children for which various explanations have been put forward. For example, it may be that increasing air pollution is predisposing patients to more frequent asthmatic attacks by increasing the hyperreactivity of the bronchial muscles.
Food allergies
Allergies to food are also seen in atopic individuals. Normally, the allergy will present as a skin rash, possibly with diarrhea, within an hour of consumption of the particular food involved. Foods known to cause allergies include eggs, shellfish, mushrooms and strawberries. Recently, much attention has focused on the extent of severe allergic reactions to nuts, especially peanuts. This may be due to the increased use of peanut paste as a thickening agent in the preparation of processed foods. Individuals who are allergic to peanuts may suffer rapid and life-threatening allergic reactions and are advised to avoid processed food unless the ingredients are clearly labeled. It has also been known for individuals to suffer severe reactions to certain fruits, such as papaya, though this is rare.
Management of Type I hypersensitivity
The most appropriate strategy for treating Type I hypersensitivity is to identify the allergen and to avoid it. Laboratory tests to identify the allergen in question may involve skin testing. Extracts of common allergens are injected intradermally. In sensitive individuals, the causative allergen will produce a ‘wheal and flare’ skin reaction within 20 min. The ‘wheal’ is a raised red lump, while the flare is the red inflamed area that surrounds it. Investigations of Type I hypersensitivity include the radioallergosorbent test (RAST) which measures the level of allergen-specific IgE in the blood. This involves incubating samples of serum from a patient with the potential allergen immobilized on a solid support, any IgE that becomes bound to the allergen is then detected by the addition of 125I-labeled anti-IgE antibodies.
When complete avoidance of the allergen is not feasible, drugs may be used to control the symptoms. These include antihistamines, such as brompheniramine maleate and loratadine, anti-inflammatory drugs, such as corticosteroids, and ‘Intal’ which prevents mast cell degranulation.
TYPE II HYPERSENSITIVITY
Type II or cytotoxic hypersensitivity refers to those situations in which antibody activates complement causing tissue damage. Examples include transfusion reactions to mismatched blood, and hemolytic disease of the newborn (HDN). In addition, autoimmune reactions that involve lysis of cells can be included here. Autoimmune diseases have already been discussed above and transfusion and HDN are described, hence only a brief discussion of the causes and consequences of the transfusion of ABO incompatible blood will be given here.
Transfusion reactions
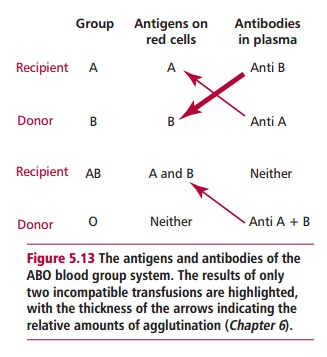
The ABO blood group system contains four blood groups: A, B, AB, or O, according to the types of antigens found on erythrocyte membranes. In the plasma, there are also antibodies to the blood group antigens thatare not present on the erythrocyte membranes. Thus, individuals with blood group A have anti-B antibodies in their plasma, while those of blood group B have anti-A (Figure 5.13). These antibodies are known as isohemagglutinins, and usually belong to the IgM class, which are efficient activators of complement. If a blood group A individual is transfused with group B blood, then antibodies from the donated blood will bind to recipient erythrocytes, activate complement and cause their lysis. Similarly, antibodies in the recipient will lyse the donated erythrocytes. The sudden and simultaneous lysis of cells leads to kidney failure and death.
TYPE III HYPERSENSITIVITY
Type III or complex-mediated hypersensitivity is brought about by immune complexes that usually involve antibodies to soluble antigens. Immune complexes can be harmful because they activate complement, triggering inflammation and the influx of neutrophils into an area. Over a period of time, this can cause tissue damage, principally due to lytic enzymes released by dying neutrophils. As the size of immune complexes varies, depending on the relative proportions of antigen and antibody, the clinical consequences may vary. For example, in autoimmune diseases such as RA immune complexes between rheumatoid factor and IgG are produced in antigen excess. These complexes are small and soluble and travel in the circulation. They may adhere to the insides of blood vessels, triggering vasculitis, or terminate in the kidney and cause nephritis. In intrinsic allergic alveolitis, immune complexes produced in the alveoli are large, and precipitate in the lungs, causing alveolitis. The name ‘intrinsic allergic alveolitis’ covers a number of
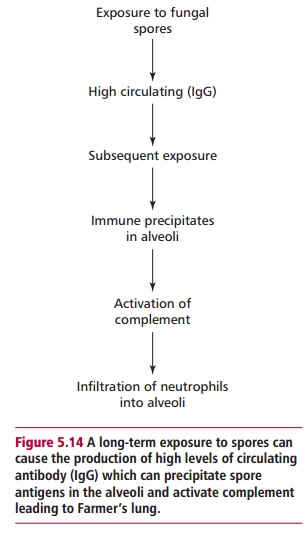
occupational diseases, in which workers are exposed to air-borne immunogens. A typical example of this disorder is Farmer’s lung (Figure 5.14). This disorder typically begins in winter time, when the farmer develops a cough. Since this is not an unusual occurrence, the disease may go unrecognized for several years. However, the disease is progressive and, if untreated, will progress to emphysema. The disease is related to the farmer moving hay to feed livestock during the winter. Ascomycete fungi grow well in the warm damp conditions at the center of a haystack, and a cloud of spores are released when the hay is moved. The farmer inhales the spores and, over months and years, develops high levels of circulating IgG to immunogenic molecules which have been leached from the spores. With high levels of IgG in the blood supply to the alveoli, further exposure to spore antigens causes large immune complexes to precipitate in the lungs, setting up inflammation in the alveoli.
Successive winters may result in immune complex-mediated damage to the lungs, with fibrosis and loss of gas exchange capacity. Although Farmer’s lung is classified as an antibody-mediated hypersensitivity, it is now recognized that cell-mediated immunity is also involved and that damage caused by specific T cells also contributes to the disease. It is essential that Farmer’s lung be diagnosed early to avoid permanent damage to lung tissue. Treatment in the early stages may simply involve avoidance of the antigen, although corticosteroids may also be used to treat the inflammatory reaction.
TYPE IV DELAYED TYPE HYPERSENSITIVITY
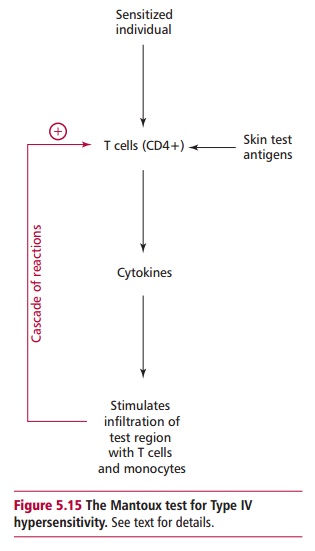
Delayed-type hypersensitivity (DTH) requires more than 18 h after exposure to an immunogen for the symptoms to become apparent. This type of hypersensitivity is caused by T lymphocytes rather than antibody. The DTH reaction is typified by the Mantoux reaction. The vaccine to protect against tuberculosis (TB) consists of an attenuated form of Bacillus Calmette Guérin (BCG) which is a strain of Mycobacterium bovis . Before being given the vaccine, individuals are skin tested to see if they are already sensitized by infection or previous vaccination. This involves injecting an extract of mycobacteria, called purified protein derivative (PPD) intradermally. If an individual is sensitized, then after about 18–24 h, the injection site becomes swollen and red. The swelling increases for around 48 h then subsides slowly so that this ‘positive’ reaction is still visible after several weeks. An individual who gives a positive Mantoux test may then be investigated to ensure that the positive result was due to prior sensitization rather than active disease.
The swelling is caused by small lymphocytes and monocytes infiltrating into the area. Initially, sensitized CD4+ T cells respond to PPD by releasing cytokines (Figure 5.15) that attract and retain monocytes at the site and induce inflammation, allowing the entry of more CD4+ cells. Thus a cascade reaction occurs, producing a slow but progressive swelling at the site of the injection. The reaction subsides once the phagocytic monocytes have removed all the PPD.
Delayed type hypersensitivity is also seen in contact allergies to a number of chemicals, including certain biological stains, some hair dyes, nickel salts in cheap jewellery, mercuric salts in some tattoo dyes, fluorodinitrobenzene and some plant biochemicals, such as urushiol in poison ivy. Typically, once sensitized, an individual will develop dermatitis approximately 18 to 24 h after further skin contact with the same chemical. Skin sensitizing chemicals are not typical immunogens, since they are neither proteins nor large molecules. However, it appears that sensitization involves their chemical binding to skin proteins to form a hapten-protein conjugate . Langerhans cells, which are antigen presenting cells in the skin, process the ‘new’ antigen and present it to helper T lymphocytes, which become sensitized. Once this has happened, any further contact with the chemical will promote cytokine release from T cells, producing a cascade similar to that of the Mantoux reaction
Laboratory workers need to be aware of the skin sensitizing nature of many of the chemicals used in biomedical science and to conduct risk assessments for their use, since sensitization, once induced, is irreversible. The only treatment for Type IV hypersensitivy is to avoid the allergen, although corticosteroid creams may give some relief during an episode of dermatitis.
Related Topics