Chapter: Medicine Study Notes : Cardiovascular
Peripheral Exam - Physical Exam
Physical Exam
·
Position patient at 45 degrees
·
General appearance, including
cachectic state, Marfan‟s, Down‟s or Turner‟s Syndromes
·
Dextrocardia = heart on right
hand side (1 in 400??). Need right-sided
heart leads
Peripheral Exam
Hands
·
Check for clubbing (congenital
cyanotic heart disease), warmth (perfusion), capillary refill, anaemia (palmar
creases), peripheral cyanosis, splinter haemorrhages
Pulse
·
Radial pulse: assess rate,
rhythm, and delay from radial to femoral pulse (radio-femoral delay)
·
Brachial or Carotid pulse:
Character and volume
·
Rate:
o Sinus Tachycardia:
§ = Sinus rhythm > 100 bpm. 120 bpm could be physiological, > 140 –
150 bpm more likely to be an aberrant rhythm
§ Causes: fever, exercise, emotion, anxiety, pain, pregnancy, anaemia,
hypoxia, thyrotoxicosis, HF, catecholamine excess, constrictive pericarditis,
myocarditis, shock, MI, drugs, smoking, coffee, autonomic neuropathy (eg in
DM), PE
o Sinus bradycardia:
§ = Sinus rhythm < 60 bpm
§ Causes: athlete, during sleep, drugs (b-blockers,
digoxin, amiodarone), hypothyroidism, hypothermia, severe jaundice (due to
bilirubin in conducting system), 3rd degree heart block, MI, paroxysmal bradycardia (eg vasovagal syncope)
·
Rhythm:
o Regular
o Irregular:
§ Irregularly irregular: usually atrial fibrillation
§ Regularly irregular: Sinus arrhythmia (rate with
respiration and ¯ with expiration) or 2nd degree heart block (Mobitz type 1)
·
Quality:
o If „thin‟ then ¯ volume
o Slow rising, low volume Þ aortic stenosis
o Radial/femoral delay Þ aortic stricture e.g. coarctation,
o Bounding pulse = a pronounced pulse – big difference between systolic
and diastolic pressure (i.e. large pulse pressure). If bounding then always do
a collapsing check
o Collapsing pulse = bounding pulse + thumping pulse felt over wrist with
palm of your hand when patient‟s arm raised - ?aortic regurgitation (higher
column of blood ® regurgitation)
·
Pulse deficit = difference
between the radial pulse rate and heart rate. If rapid or irregular contraction
then no time for ventricular filling Þ there may not be a corresponding
radial pulse beat
Measuring Blood Pressure
·
Ways of measuring blood pressure:
o Mercury sphygmomanometer: listen for Kortokoff sounds
o Oscillotonometer: detects arterial pulsations transmitted by the cuff.
Tend to over-read very low pressures (oscillations diminish in amplitude)
o Ultrasound sphygmomanometer: uses Doppler shift
o Direct measurement: intra-arterial pressure with transducer
·
How to measure with a
sphygmomanometer:
o Patient relaxed/seated for 5 minutes
o Arm at heart level
o Hold their hand under your right arm, straighten their arm and support under elbow. Use right thumb to feel brachial pulse as cuff is inflated (so you don‟t over-inflate). Inflate to 30 mmHg above point where pulsation stops
o Don‟t push stethoscope diaphragm too hard (otherwise ® bruit)
o Start of Kortokoff sound 1 = systolic.
Disappearance of Kortokoff sound 5 = diastolic
o In obese people a normal width cuff will over-estimate blood pressure –
must use a large one
o Repeat several times, and on several occasions before deciding to treat
o Sources of operator error:
§ Wrong sized cuff
§ Poor positioning of the patient
§ Too rapid release of cuff pressure
§ Use of non-standard diastolic end points
§ Rounding to 5‟s or 10‟s
·
Watch for:
o Pulsus paradoxus: Normally inspiration ® ¯systolic
and diastolic blood pressure (more negative intrathoracic pressure ® pooling
in pulmonary vessels ® ¯filling). Pulsus paradoxus = this decrease is exaggerated (ie fall of
> 10 mmHg). Can occur in constrictive pericarditis, pericardial effusion or
severe asthma
o Postural hypotension:
§ Fall of more than 15 mmHg systolic or 10 mmHg diastolic on standing
§ Causes: hypovolaemia, drugs (vasodilators, antidepressants, diuretics), Addison‟s
disease, hypopituitarism, autonomic neuropathy
§ Pulse on
standing. For vasovagal syncope pulse ¯
· Hypertension
Face
·
Eyes:
o Jaundice from liver congestion secondary to heart failure
o Anaemia
o Roth‟s spots on retina: areas of retinal infarction and haemorrhage
caused by septic emboli in bacterial endocarditis
·
Xanthelasma: intracutaneous
yellow cholesterol deposits around the eye. Normal variant or ?hyperlipidaemia
·
Mitral facies: rose cheeks with
dilated blue veins and cyanosed tongue. Due to pulmonary hypertension and ¯cardiac
output (eg as in severe mitral stenosis)
·
Mouth: diseased teeth (cause of
infective endocarditis), tongue for central cyanosis, and mucosa for petechiae
Carotid Arteries
· Information about aorta and left ventricular function ,
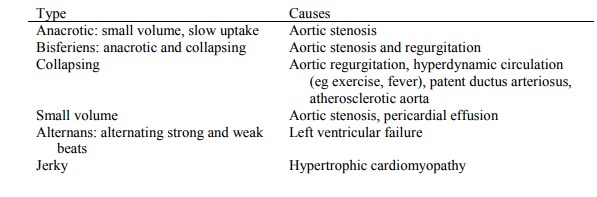
Pulse wave forms:
Jugular Venous Pressure (JVP)
·
Information about right atrial
and right ventricular function
·
in RVF, volume overload, impaired RV filling, SVC syndrome
·
Positioning:
o Patient should be at 45 degrees
o Internal jugular is medial to the superior end of sterno-mastoid then
runs behind it as it descends
o External is lateral, is easier to see, but is more tortuous and therefore less reliable
o Sternal angel is the zero point – pulsations are visible above this
point at 45 degrees (centre of the right atrium is 5 cm lower). Normal is
pulsations just above the clavicle (+3 cm)
·
Differentiating from carotid pulse. The JVP is:
o Visible but not palpable
o Flickers twice with each cardiac cycle
o Usually decreases with respiration
o Is obliterated then filled from above following light pressure at the
base of the neck
·
Pressure waves in atria:
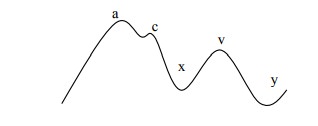
o a wave: atrial contraction at end of diastole ® atrial
pressure. Coincides with first heart sound and precedes carotid pulse. Closely
followed by …
o c point: bulging of AV valves into atria during systole ® atrial
pressure. Not usually visible
o x descent: atrial relaxation between S1 and S2
o v wave: End of atrial filling during systole – venous inflow into atria
with AV valve closed ® atrial pressure
o y descent: rapid ventricular filling following opening of the AV valve
·
Height (the easy bit – ha ha!):
o If > 3 cm above the zero point then right heart filling pressure is
raised
o Rises with 10 seconds pressure on the liver (hepatojugular reflex). A
rise is normal. If it remains raised then ventricular failure
o Causes of height: Right ventricular failure, tricuspid stenosis or regurgitation,
pericardial effusion or constrictive pericarditis, SVC obstruction (no waves),
fluid overload, hyperdynamic circulation
o Should normally fall on inspiration. If it rises then ?constrictive
pericarditis. Investigate with echo
·
Character (the hard part):
o Causes of a dominant a wave: tricuspid stenosis (also causes a slow descent), pulmonary stenosis, pulmonary hypertension
o Causes of cannon a waves (wave - right atrium contracts against closed tricuspid valve): intermittently in complete heart block (two chambers beating independently), retrograde conduction
o Cause of dominant v wave: tricuspid regurgitation (should never miss
this, watch for movement of ear lobe)
o x descent: absent in AF, exaggerated in cardiac tamponade, constrictive
pericarditis
·
y descent: Sharp: severe
tricuspid regurgitation, constrictive pericarditis, slow in tricuspid stenosis,
right atrial myxoma
Related Topics