Chapter: Medicine Study Notes : Cardiovascular
Arrhythmias
Arrhythmias
· For cardiac arrest rhythms (VT, VF, Torsade and asystole)
Atrial Fibrillation
· = a type of supra-ventricular arrhythmia
· Mechanism:
o Wave of depolarisation circulates in atria at much faster rate than the discharge from the SA node. Disorders changing the conduction characteristics of the AV node predispose to AF: atrial size, fibrosis, inflammation, thyrotoxicosis, ischaemia, altered autonomic tone, alcohol use, after bypass surgery (30%), after valve replacement surgery (50%)
o AV node receives irregular impulses at a rate of 250 – 400 per minute. Conducted through the node at a frequency dependent on the pathway‟s refractory period
o Typical ventricular rate is 120 per minute: but this may if sympathetic stimulation (® ¯refractory period) or alternative conducting path to the AV node (eg Wolf-Parkinson-White syndrome)
· Epidemiology: most common cardiac arrhythmia. M > F. 5% of over 70s
· Causes:
o IHD: especially post MI
o Mitral valve disease
o Alcohol
o Thyroid disease
o Idiopathic
· Potential implications:
o Thrombo-embolism: Especially cerebral (also mesenteric arteries or lower limbs). If no other risk factors then 1% per year. 5% if one other risk factor (age over 65, BP, heart failure, diabetes, IHD, previous embolism, RF). If RF and AF then 20% annual rate
o Reduced cardiac output: ¯Ventricular filling ® ¯Cardiac output ® heart failure or ¯exercise tolerance. Also high ventricular rate ® ¯filling ® ¯CO
o Other symptoms: palpitations (25%) and dizziness or syncope (20%)
· Diagnosis: should always be confirmed by ECG. Ventricular rhythm in AF can be deceptively regular, and not all irregular rhythms are AF (eg variable AV block, ventricular or atrial ectopics)
· Assessment:
o Exclude thyrotoxicosis
o Manage contributing MI, respiratory disease or alcohol abuse
o Check electrolytes
o Assess cardiovascular risk factors: eg glucose, lipids
o Echocardiogram to assess atrial size or abnormal ventricles (eg valvular heart disease). These are harder to cardiovert (also have a higher risk of embolism). Echocardiogram is poor at detecting thrombis (trans-oesophageal echocardiogram is better)
· Management:
o Cardioversion: indicated if onset is within 24 – 48 hours and no other risk factors (eg no atrial enlargement or ventricular abnormality). Involves general anaesthetic and synchronised DC shock at 100 then 200J. Successful in about 85%. May need anticoagulation for cardioversion (thrombi may get dislodged if normal rhythm returns).
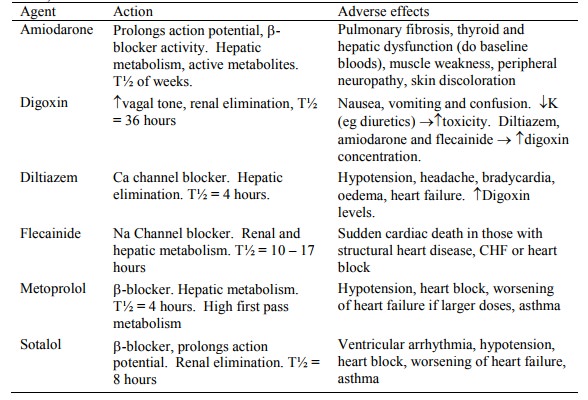
o Chemical cardioversion: flecainide and amiodarone – successful in 60 – 90%. (Digoxin does not cardiovert)
o > 50% revert in one year if no ongoing drug treatment
· Drug treatment: consider digoxin (increases heart block ® slows ventricle ® improved pump action), flecainide (in those without structural heart disease), Amiodarone (extensive toxicity issues) or Sotalol:
o Antithrombotic therapy: Reduces annual risk in those at risk from 5% to 1.5% (60% relative risk reduction), with 1% having material anti-coagulant side effects. Use warfarin with a goal of an INR from 2 to 3. Use aspirin if warfarin contra-indicated (only 10 – 15% relative risk reduction)
· Atrial flutter: probably due to atrial re-entry. Regular atrial saw tooth pattern with ventricular beat every 3:1 or 4:1. If unstable hypotension, synchronised counter-shock at 50J (treat as for AF)
Sinus Arrhythmia
· Normal sinus rhythm: rate 60 to 100 per minute, P wave upright in leads I, II and AVF
· Sinus tachycardia:
o discharge of sinus node. Rate is > 100/minute and regular
o P wave is upright in leads I, II, AVF. Treat underlying cause
· Sinus bradycardia:
o Constant and normal PR interval
o < 60 bpm: but this is relative. An athlete may normal at 40, and a hypovolaemic patient bradycardic at 65 bpm
o Causes: SA node disease, parasympathetic tone, drug effect
o Treat if hypotension or ventricular escape beats present
o Treatment: atropine (0.6 mg) unless MI, transthoracic pacing, dopamine or adrenaline
· Sick Sinus Syndrome: Common in elderly. Bradycardia +/- arrest, AV block, or SVT alternating with bradycardia/asystole (Tachy-Brady Syndrome). Pace if symptomatic
Other Abnormal Rhythms
· Atrial tachycardia (paroxysmal atrial tachycardia) – SVT (Supraventricular Tachycardia):
o Narrow QRS complex (always exclude atrial flutter with 2:1 block)
o Often abrupt onset, last for seconds to many hours, then abrupt offset
o Rate is usually 160 – 200/min
o Therapy: vagal stimulation (carotid massage, one side at a time), adenosine, amiodarone, beta-blockers or digoxin. If LV failure, chest pain or HR > 220 bpm then synchronised counter-shock
· Premature Atrial Complexes (PAC): atrial ectopic beats. Small spike before premature but normal width QRS
· Junctional or Nodal rhythm: regular rhythm. May be no detectable P wave (due to retrograde firing into atrium) or inverted P-wave with short PR interval. P wave may be buried in QRS complex. Rate of 40 – 60 bpm. Reduction in atrial filing. Treatment often not indicated
· Premature Ventricular Complexes (PVC‟s): bizarre, wide QRS complexes triggered by an ectopic ventricular focus. Most common post-MI rhythm. Unifocal PVC‟s (each complex looks the same) or multifocal (each complex looks different from others)
Heart Block
· Atrioventricular block/Heart Block: Delay or interruption in conduction between atrium and ventricle
o First degree (partial block): PR interval prolonged beyond 0.2 secs (5 small squares). Often seen in normal people. ?Acute MI or Rheumatic Fever. No urgent action needed.
o Second degree AV block (partial block): some impulses are conducted and some not. Þ Heart disease. Often seen in acute MI:
§ Mobitz type 1 (Wenckebach): progressive prolongation of PR interval before an impulse is completely blocked – then sequence starts over. Usually transient and prognosis is good
§ Mobitz type 2: PR interval does not lengthen but some beats are not conducted. May lead to bundle branch block (® wide QRS), transvenous pacing may be required
§ 2:1 block (every second beat gets through). Also 3:1 block. May need pacing if ventricular rate too slow.
o Third degree (complete heart block): no conduction – either at AV, bundle of His or bundle branch level. More often fibrosis than ischaemia:
§ At level of AV node: junctional escape pacemaker will fire at 40 – 60 bpm with normal QRS. Prognosis favourable. Due to parasympathetic tone from inferior MI or drug effect
§ At infranodal level: Implies extensive disease of both bundles. Associated with anterior MI. Distal escape rhythm, slow rate (<40) plus wide QRS, possibly asystole. Management: transvenous or transthoracic pacing, dopamine or adrenaline, pacemaker
Drugs for Acute, Life Threatening Arrhythmias
· For tachycardias:
o Ventricular Tachycardia:
§ Lignocaine: dose 1 – 1.5 mg/kg by slow iv bolus, followed by infusion of 1 – 4 mg/min. Reduce dose in heart failure, shock, > 70 years, b blockade & hepatic disease. Side effects include convulsions. Action on sodium channels reduces myocardial excitability, especially in ischaemic myocardium. Raises threshold for VF, and suppresses VT and ventricular ectopy. Should be considered in VF after 3 defibrillatory loops. No evidence of usefulness in converting VF but may prevent return to VF. Reduces blood pressure and slows the heart rate
§ Bretyllium: anti-adrenergic, although initially causes adrenergic stimulation (for 20 minutes), raises VF threshold. Use if lignocaine fails
§ Procainamide: powerful antiarrhythmic and strong negative inotropic agent, but slow to act. Use where lignocaine has failed to suppress recurrent ventricular tachycardia
§ Magnesium: prevention and treatment of refractory ventricular arrhythmias
o SVTs:
§ Adenosine: slows sinus rate and AV conduction. Use for SVT due to re-entry. Very short T½
§ Verapamil: Ca blocker. Suppresses pacemaker activity in SA and AV nodes. For SVT where adenosine has failed
§ Amiodarone: delays repolarisation with less cardiac depression than other antiarrhythmics. Good for SVT, less so for ventricular arrhythmias. Via central line, long T½
§ b-blockers: useful in treatment of hypertension, supraventricular arrhythmias and recurrent VT where LV function is not severely impaired. E.g. propranolol (unselective), atenolol (b1 selective), metoprolol (relatively b selective), labetalol (a & b selective, short acting, for acute hypertensive crises), sotalol (non-selective b blocker + antiarrhythmic), esmolol (ultra-short acting b block)
· For bradycardias:
o Atropine: Competitive anticholinergic at muscarinic nerve endings. Enhances SA discharge and AV conduction. Use in bradycardia or AV block. Care in MI – may increase pulse ® extension of ischaemia
o Isoprenaline: b agonist - use for significant bradycardia refractory to atropine. Use dopamine or adrenaline first
· Other supra-ventricular arrhythmias:
o Digoxin: force of contraction and ¯AV conduction – for heart failure and supraventricular arrhythmias (particular AF). Avoid in recent MI, heart block, renal impairment, and hypokalaemia
o Dopamine: for treatment complete heart block. A catecholamine. Infuse at 5 – 20 mg/kg/min. Adjust to keep heart rate at 60 beats per minute. renal blood flow (® renal output) through renal vasodilator and due to CO and perfusion generally
· Others:
o Inotropes: dopamine and dobutamine – for supporting blood pressure once cardiac output has been established. Useful in cardiac failure secondary to ischaemia.
o Nor-adrenaline: intense vasoconstrictor – use for restoring MAP where vasodilation induced hypotension
o GTN: venous vasodilator - ¯blood pressure and improve artery blood flow. Preload and afterload reduced
o Diuretics: frusemide – also causes venodilation (® ¯preload)
o Antihistamines: H1 antagonists (promethazine / Phenergan), H2 antagonists (ranitidine)
Emergency cardiac pacing
· Complete heart block most common indication. Also for non-response bradycardias and asystole with P waves
· Transcutaneous/transthoracic pacing: Electrodes over apex and sternum. Sedation + analgesia required. Temporary measure only
· Transvenous pacing: via arm or neck vein into right atrium or ventricle
Cardiac Arrest Rhythms
· See also Arrhythmias(Topic)
· Due either to:
o Disordered electrical activity (arrhythmia) such as following an MI, or
o Impaired mechanical performance: Pulseless Electrical Activity (PEA) or Electro-Mechanical Dissociation (EMD) – primary (damaged myocardium, e.g. ischaemia) or secondary (e.g. hypovolaemia, pneumothorax, anaphylaxis ® ¯afterload, pulmonary embolus). EMD has worst prognosis. ECG may be normal but patient is still arresting
· Ventricular Fibrillation (VF)
· Most non-traumatic arrests are ventricular fibrillation. Only effective treatment is defibrillation
· No organised depolarisation ® doesn‟t contract as a unit. But still contracting Þ still using O2
· Coarse VF: irregular, large amplitude ECG waves ® onset recent. Responds well to defibrillation (if given within 5 – 8 minutes). CPR not sufficient to maintain the coronary artery perfusion necessary to offset O2 consumption ® rapid ischaemia. Precordial thump MAY revert VF
· Fine VF: progressively lower amplitude VF until indistinguishable from asystole. 5-10% decrease in likelihood of successful defibrillation per minute
· Treatment:
o Defibrillation
o CPR and adrenaline help maintain diastolic BP and thus cardiac perfusion
o If failing, consider sodium bicarbonate and lignocaine (antiarrhythmic)
o Discontinue after 30 minutes
· Ventricular Tachycardia
· Fast (100 – 220/minute) and wide QRS complexes (> 0.12 sec)
· Causes: ischaemia, K or Mg disturbances, PE, etc
· Can be confused with supraventricular tachycardia with bundle branch block
· Dangerous precursor of VF
· Treatment:
o If stable (i.e. still sufficient cardiac output ® pulse):
§ Oxygen
§ Lignocaine (1 mg/kg) stat plus 0.5 mg/kg every 8 minutes up to 3 mg/kg
§ If this fails then cardioversion
§ If little cardiac output/no pulse: same as for VF
o If pulse but unstable:
§ Sedation
§ Cardioversion: starting at 50J, then 100 then 200 then 300. If recognisable regular rhythm then synchronised
§ If recurrent, give lignocaine, then procainamide 20 mg/min up to 1000 mg then bretyllium 5 – 10 mg/kg and magnesium
· Torsade de Pointes
· ECG like VT – but QRS amplitude changes due to rotating electrical axis
· May be self-limiting for periods of 5 – 10 secs
· May be due to anti-arrhythmics prolonging the QT interval (if so, stop them)
· Treat by correcting electrolyte abnormalities and by increasing basic heart rate (i.e. over-pacing)
· Magnesium sulphate 1-2gms given over 1 – 2 minutes may reverse drug induced torsade
· Defibrillate for sustained episodes or use over-drive pacing
· Asystole
· Complete absence of ventricular electrical activity
· Usually end result of major disturbance/myocardial damage
· Usually a wandering straight line (if completely flat check ECG)
· Invariably fatal after 15 minutes
· Atropine + CPR may bring back rhythm
Related Topics