Chapter: Medicine Study Notes : Cardiovascular
Atrial Fibrillation - Arrhythmias
Arrhythmias
· For cardiac arrest rhythms (VT, VF, Torsade and asystole)
Atrial Fibrillation
·
= a type of supra-ventricular
arrhythmia
·
Mechanism:
o Wave of depolarisation circulates in atria at much faster rate than the
discharge from the SA node. Disorders changing the conduction characteristics
of the AV node predispose to AF: atrial size, fibrosis,
inflammation, thyrotoxicosis, ischaemia, altered autonomic tone, alcohol use,
after bypass surgery (30%), after valve replacement surgery (50%)
o AV node receives irregular impulses at a rate of 250 – 400 per minute.
Conducted through the node at a frequency dependent on the pathway‟s refractory
period
o Typical ventricular rate is 120 per minute: but this may if sympathetic stimulation (® ¯refractory period) or alternative conducting path to the AV node (eg Wolf-Parkinson-White syndrome)
·
Epidemiology: most common cardiac
arrhythmia. M > F. 5% of over 70s
·
Causes:
o IHD: especially post MI
o Mitral valve disease
o Alcohol
o Thyroid disease
o Idiopathic
·
Potential implications:
o Thrombo-embolism: Especially cerebral (also mesenteric arteries or lower
limbs). If no other risk factors then 1% per year. 5% if one other risk factor
(age over 65, BP, heart failure, diabetes, IHD, previous embolism, RF). If RF and AF
then 20% annual rate
o Reduced cardiac output: ¯Ventricular filling ® ¯Cardiac output ® heart failure or ¯exercise tolerance. Also high ventricular rate ® ¯filling ® ¯CO
o Other symptoms: palpitations (25%) and dizziness or syncope (20%)
·
Diagnosis: should always be confirmed by ECG. Ventricular rhythm in AF can be
deceptively regular, and not all irregular rhythms are AF (eg variable AV
block, ventricular or atrial ectopics)
·
Assessment:
o Exclude thyrotoxicosis
o Manage contributing MI, respiratory disease or alcohol abuse
o Check electrolytes
o Assess cardiovascular risk factors: eg glucose, lipids
o Echocardiogram to assess atrial size or abnormal ventricles (eg valvular
heart disease). These are harder to cardiovert (also have a higher risk of
embolism). Echocardiogram is poor at detecting thrombis (trans-oesophageal
echocardiogram is better)
·
Management:
o Cardioversion: indicated if
onset is within 24 – 48 hours and no other risk factors (eg no atrial
enlargement or ventricular abnormality). Involves general anaesthetic and
synchronised DC shock at 100 then 200J. Successful in about 85%. May need
anticoagulation for cardioversion (thrombi may get dislodged if normal rhythm
returns).
o Chemical cardioversion: flecainide and amiodarone – successful in 60 –
90%. (Digoxin does not cardiovert)
o > 50% revert in one year if no ongoing drug treatment
·
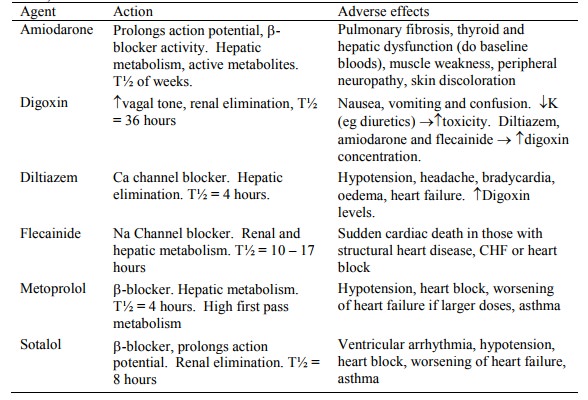
Drug treatment: consider digoxin
(increases heart block ® slows ventricle ® improved pump action), flecainide (in those without structural heart
disease), Amiodarone (extensive toxicity issues) or Sotalol:
o Antithrombotic therapy: Reduces annual risk in those at risk from 5% to
1.5% (60% relative risk reduction), with 1% having material anti-coagulant side
effects. Use warfarin with a goal of an INR from 2 to 3. Use aspirin if
warfarin contra-indicated (only 10 – 15% relative risk reduction)
·
Atrial flutter: probably due to
atrial re-entry. Regular atrial saw tooth pattern with ventricular beat every
3:1 or 4:1. If unstable hypotension, synchronised counter-shock at 50J (treat
as for AF)
Related Topics