Chapter: Medicine Study Notes : Cardiovascular
Ischaemic Heart Disease
Ischaemic Heart Disease
·
Most common cause of death in
Western countries
·
Incidence peaked in NZ in 1968 at
320 deaths /100,000. Now 200/100,000
·
In NZ, 4,500 acute MI per year,
3,200 CIHD per year (=25% of all deaths)
·
Risks factors:
o Cigarette smoking 5.2 x
o Hypertension 3.3 x
o Hyperlipidaemia 3.7 x
o Diabetes mellitus
o Male gender
o Family history
·
Pathogenesis
o Myocardial blood flow < metabolic demand of myocardium
o Coronary perfusion related to:
§ Atherosclerosis occluding coronary arteries (fixed coronary stenosis),
acute plaque changes (eg rupture), thrombosis, vasoconstriction
§ Differential between ostia (aortic diastolic pressure) and coronary
sinus (right atrial pressure)
§ Compression of intramuscular arteries during contraction ®
myocardium perfused in diastole
§ Decreased coronary blood flow also due to intraventricular
pressure & myocardial contraction, aortic valve stenosis/regurgitation, right
atrial pressure
·
Cross sectional area of major
vessels must be reduced by 75% to significantly affect perfusion
Hypertension
· See Measuring Blood Pressure(Topic), for measurement
·
Is a risk factor not a disease
·
Definition:
o No dividing line between normal and high blood pressure. There are
arbitrary levels set based on the risk of complications (the main ones being
stroke, MI, heart failure and renal failure)
o In determining whether the blood pressure is „bad‟, take into account
the systolic and diastolic pressure, age, sex, other diseases (eg DM,
hyperlipidaemia), smoking. Older age is the greatest risk factor: treat high
blood pressure in an older person regardless of other risk factors
o WHO definitions:
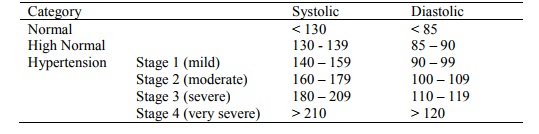
o Also classified according to retinopathy, see Hypertensive Retinopathy(Topic)
·
Classified as:
o Primary/essential (what most people have – but a diagnosis of
exclusion): contributing factors include hereditary, obesity, alcohol intake,
salt intake (60% of patients respond to ¯salt intake – but compliance
difficult)
o Secondary causes: renal disease (eg renal artery stenosis, diabetic
kidney disease, etc), endocrine (eg cortisol, aldosterone,
acromegaly, oral contraceptives), neurogenic (eg psychogenic), sleep apnoea
(major changes in baroreceptor reflexes)
·
Epidemiology:
o Prevalence with age. Older people at greater risk at any given blood pressure
compared with young
o Strong risk factor for stroke, congestive heart failure, coronary artery
disease and renal failure
o Probably 10 – 20% of older adults require treatment (ie have essential
hypertension with diastolic pressure > 95 mmHg)
o Treatment reduces related complications. Stroke risk reduces in line
with BP, MI risk doesn‟t reduce as much for a given drop in BP
·
History:
o How accurate is the diagnosis?
o Usually symptomless
o Possibly related symptoms: palpitation, flushing, headache
o Related risk factors: history of renal, cardiac or neurological disease
o Asthma, diabetes, gout, renal disease: complications with drug treatment
o Occupational
o Diet: salt, fat
o Smoking and alcohol
o Family History
·
Detection and assessment:
o Blood pressure more labile in older adults Þ measure
2 to 3 times (in same arm). Measure standing and sitting
o In primary hypertension usually on standing. In secondary hypertension, usually ¯ on
standing
o Basic workup:
§ Urine for protein, blood and glucose ® DM, renal disease
§ FBC for polycythaemia, renal disease, alcohol
§ Electrolytes (especially K): exclude odd endocrine causes
§ ECG: any end organ damage
o Additional tests if indicated:
§ Microscopic analysis of urine (for casts)
§ Plasma lipids
§ Blood glucose: need to modify drug treatment
§ Serum Ca, PO4, uric acid (gout – associated with hypertension, may also due to
drugs)
§ Echocardiogram or CXR
§ Special tests for secondary causes if indicated: eg renal imaging, 24
hour urine for catecholamine metabolites (phaeochromocytoma)
·
Pathology:
o Pathophysiology: poorly understood. Older people have ¯renin,
and are more responsive to Na depletion. „Hardening‟ of arteries ®systolic
pressure. ¯Responsiveness to b-mediated vascular relaxation
o Leads to hypertensive heart disease: left ventricular hypertrophy ® relative
myocardial ischaemia. Aortic valvular disease also ® LV
hypertrophy
o Malignant hypertension (accelerated hypertension): hypertension leading
to rapidly progressive vascular compromise. Blood vessels show fibrinoid
necrosis or concentric hyperplasia („onion skin‟ changes)
Non-drug treatment
·
Remove/substitute drugs: eg
NSAIDs, OCP, Prednisone
·
Always attempt lifestyle changes
first:
o Stop smoking (little effect on BP, but biggest impact on risk factors)
o Weight loss
o ¯Alcohol
(max 2 drinks per day)
o ¯Salt
intake (max 70 mmol/day)
o exercise
o ¯Saturated
fats
Drug Treatment
·
When to treat:
o Given it is such a strong risk factor, consider hypertension above
systolic 140 mmHg
o Always treat > 170 systolic or > 110 diastolic
o Hardly ever treat < 140 and < 90 diastolic
o In between, controversial. Consider other risks. If over 65 no other risk factors needed (eg diabetes, etc). Give considerable attention to non-pharmacological approaches for 3 – 6 months. Long term follow up necessary
o Treat 72 older adults for 5 years to prevent 1 death, treat 43 for 5 years to prevent one cerebrovascular event
o Aim of treatment: diastolic < 90
·
Rules of thumb:
o Use low doses of several agents, rather than increasing doses of one drug (especially thiazides)
o First line: thiazides (with or without a potassium sparing agent) and/or b-blocker (atenolol most used in trials). If tolerate them both then add them together
o ACE inhibitors: not so effective but rated best quality of life
o Don‟t take diuretic, ACE inhibitor and NSAIDS together (renal side
effects)
o Introduce slowly, monitor for symptoms and postural hypotension
o Aim for 140/90, and then attempt back titration 3 monthly
·
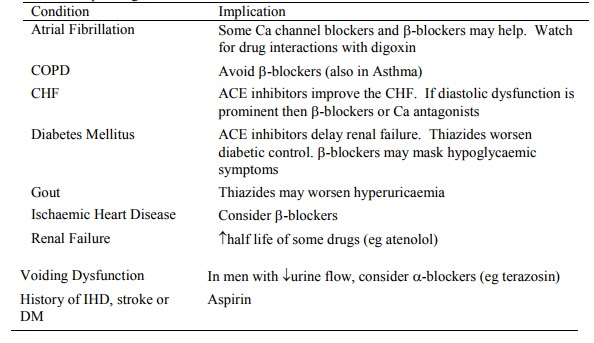
Individualise depending on
co-morbid conditions:
Angina Pectoris
·
Symptom complex characterised by
attacks of chest pain, causing ischaemia but not infarction
·
Patterns:
o Stable angina (typical): pain on exertion, relieved by rest or
vasodilators. Subendocardial ischaemia with ST-segment depression
o Variant or Prinzmetal‟s angina: classically occurs at rest. Caused by
reversible spasm in normal to severely atherosclerotic coronary arteries. Can
see ST-segment elevation or depression
o Unstable angina: variable, prolonged pain, pain at rest or worsening of pain in stable angina. ST- segment depression – but may be elevated. Most common complication: arrhythmias (especially VF). Within 3 months 4% will have sudden death and 15% a myocardial infarct
o Sudden cardiac death. Usually within an hour of a cardiac event or
without symptoms. Usually high-grade stenosis. Usually associated with
arrhythmias, especially ventricular ectopic beats and subsequent VF
·
Treatment options for stable
angina:
o Nitrates: short & long acting
o b-blockers
(¯myocardial O2 consumption)
o Ca antagonists
o Aspirin
·
Unstable angina:
o = Acute Coronary Syndrome (ACS) = acute heart problems without ST elevation
o Investigations:
§ ECG. Serial or continuous if high
risk
§ Bloods: Troponin (repeat after 6 hours), FBC, Cr, electrolytes, CK,
blood glucose. Want to test lipids/cholestrol – but false positives following
an acute coronary event. Do later.
§ CXR: cargiomegaly? Pulmonary
oedema? Dissection?
o Medical therapy:
§ Aspirin: reduces progression to MI. Neither Warfarin nor Heparin confers
little further benefit. Use heparin if high risk.
§ b-blockers:
reduce progression to MI
§ iv nitroglycerine for symptomatic relief
§ Maybe calcium channel blockers that reduce the heart rate
o Low risk:
§ Normal ECG and no detectable troponin despite angina
frequency or severity
§ Management: discharge for outpatient assessment
o High risk:
§ If even a minor degree of ST depression or a significant elevation of
troponin ® minor myocardial damage so now is the time to act
§ Overlap between High Risk ACS and non-STEMI (non-ST elevation MI)
§ Management: Admit for coronary angiography and, if positive, early
percutaneous coronary intervention (ie more aggressive treatment than
previously)
·
Long term management:
o ¯Obesity,
diabetes, smoking, exercise
o Referral to a cardiac rehabilitation programme
o Statins if serum cholesterol raised
o ACE inhibitors if hypertension or diabetes
Myocardial Infarction (MI)
Definition and Classification
·
Old WHO definition: two out of
three of: chest discomfort for > 30 minutes, enzyme rise and typical pattern
of ECG involving the development of Q waves (ie normal ECG does not rule out
infarction)
· New definition: Blood levels of sensitive and specific markers are raised in the clinical setting of acute ischaemia (ie importance of biochemical tests). See Laboratory Diagnosis(Topic)
·
2 classifications:
o ST elevation MI verses none (ie STEMI and non-STEMI). Often ST elevation
progresses to Q wave
o Q wave verses none (older classification) Þ
transmural or not
Epidemiology
·
Same risk factors as for
atherosclerosis
·
5% occur under age 40, 45% over
age 65
·
Oestrogen protective in women
pre-menopause
·
30% mortality with 20% dying
before admission
Symptoms
·
Crushing chest pain (absent in
15% of cases). But < 25% with chest
pain have an MI
·
Can also present as epigastric,
arm, wrist, or jaw discomfort with exertion or at rest
·
May be associated with dyspnoea,
sweating, nausea, vomiting, weakness, dizziness, fainting
Pathogenesis
·
Irreversible damage in 20 – 40
minutes
·
Occlusive intracoronary thrombus,
overlying ulcerated or stenotic plaque:
o Causes 90% of transmural acute MIs.
o For blood to clot need: abnormal flow, damage to vessel wall and
clotting factors.
o Thrombis formation: activated platelets adhere to exposed collagen of
damaged endothelium ® release thromboxane A2 ® expanding platelet mass + coagulation
·
Vasospasm: with or without
atherosclerosis. Postulate where no findings at post-mortem (10%) – but many of
these will be thrombi that have lysed
·
Emboli: from left sided mural
thrombosis, vegetative endocarditis
·
Arteritis: polyarteritis nordosa,
Kawasaki disease
·
Other: dissecting aneurysm
occluding coronary ostia, ¯O2 supply (anaemia, CO, cyanide), O2 demand (hyperthyroidism, fever)
Gross Morphology
·
Transmural infarct: entire
thickness of wall from endocardium to epicardium. Usually Anterior wall (50%)
or posterior free wall/septum in 15 – 30%. Q wave
·
Subendocardial infarct:
multifocal necrosis confined to inner 1/3 to ½ of left ventricle wall. More
commonly associated with temporary hypoperfusion (eg shock). No Q wave
·
Occlusion:
o LAD: 40 – 50%
o RCA: 30 – 40%
o LCA: 15 – 20%
·
Gross changes over time:
o 18 – 24 hours Pallor
of myocardium – anaemic, grey brown (cf normal brown-red)
o 24 – 72 hours Pallor
(yellow/brown) with increasingly defined hyperaemia border
o 3 – 7 days Hyperaemic border (darker brick red)
with central yellowing,
·
haemorrhagic areas
o 10 – 21 days Maximally
yellow and soft with vascular margins (red edge – granulation
·
tissues moves in)
o 7 weeks White fibrosis
Microscopic Appearance
o C – 3 hours Wavy
myocardial fibres
o 2 – 3 hours Staining
defect with tetrazolium
o 4 – 12 hours Coagulative
necrosis with loss of cross striations, oedema, haemorrhage,
·
early neutrophil infiltrate (WBCs with multilobed
nuclei), loss of
·
myocardial striations
Laboratory Diagnosis
·
Troponins:
o Increases highly specific for MI injury – but not synonymous with MI or
ischaemia, but probably indicates irreversible injury
o Increases above the 99th percentile are significant (lower than previously)
o Prognosis related to degree of elevation
o Rises no faster than CK (ie starts to rise within 3 – 12 hours) and more
expensive but substantial rise after MI (400 fold)
o Causes besides MI:
§ Subendocardial injury from wall stress in left ventricular hypertrophy
(eg heart failure)
§ Right ventricular injury in severe PE
§ Direct trauma (eg contusion)
§ Toxic injury by drugs or in septic shock
§ Myocarditis
§ Cardioversion
o Troponin T
§ = Cardiac troponin T, cTnT, TnT: only available from Boehringer Mannheim
§ Normal < 0.03 mg/l
§ Increases in renal failure due to ¯clearance (Þ false
positive)
o Troponin I:
§ Everyone else‟s test. Normal
value depends on which assay is used
§ I remains elevated for 5 – 9 days and T for 2 weeks. Better marker for
recent MI than LDH. Harder to interpret in re-infarct – don‟t know whether it‟s
the 1st or 2nd infarct
o Test on admission to either see if already raised (poor prognosis) or to
establish baseline
·
CK – total: not specific to
myocardial injury. Do baseline and use to check for reinfarction (Troponins not
so good for this)
·
Older tests:
o CK – MB fraction:
§ MM fraction is in both skeletal and myocardial muscle. But 15 – 40% of
cardiac CK is MB, compared with 2% skeletal. BB found in brain, bowel and
bladder. The MB fraction is therefore very specific
§ MB fraction rises within 2 – 8 hours. Dissipates within 1 – 3 days. So
also a good marker of reinfarction
§ CK – MB isoforms: Ratio of isoform 2 to isoform 1 > 1.5 Þ early
acute MI (changes before CK- MB elevated). Requires electrophoresis, so labour
intensive. False positives with heart failure
o Myoglobin: Oxygen binding protein in skeletal and cardiac muscle.
Elevated before CK-MB, but is not specific to cardiac muscle. Negative
myoglobin can help rule out MI
o LDH: supplanted by other tests. Rises later (24 – 48 hours) and elevated
for 7 – 14 days. Isoenzyme measurement of LDH 1 and 2 necessary for cardiac
specificity
o AST and ALT: intermediate timing but rather non-specific
· Other Investigations: CXR, echo, ABG, FBC, ?perfusion scan, ?amylase <
Management
·
Exclude differentials:
o Aortic dissection
o Pericarditis
o PE or other causes of pleuretic chest pain
o Peptic ulcer
· Investigations as for Unstable Angina(Topic)
· They will be frightened. Reassure. > 90% survival if low risk (< 60, no diabetes, no past history, pulse <100)
·
High flow O2 (unless CO2
retaining)
·
Morphine 5 – 15 mg iv at < 1
mg/min (+ antiemetic eg metoclopramide 5 – 10 mg iv). Effects: analgesic,
anxiolytic, anti-arrhythmic, venodilatory
·
Restoring/Maintaining vessel
patency:
o Aspirin 300 mg (unless contra-indicated)
o Thrombolysis:
·
Indicated if with 12 hours of MI
·
Best within 60 mins
·
Contraindications:
o General bleeding tendency: warfarin, haemophilia, severe liver disease,
thrombocytopenia
o Local bleeding risk: Past haemorrhagic stroke or recent surgery,
prolonged resuscitation (® rib fractures, contusion, etc), peptic ulcer, GI bleeding, pregnancy,
cavitating Tb
o Severe hypertension (systolic > 200, diastolic > 120)
o Pre-existing thrombis that might embolise (eg endocarditis, aortic
aneurysm)
·
Options:
o Streptokinase: restores perfusion in 30%
o TPA: restores perfusion in 54%. Expensive. Use tPA if previous reaction
to SK, or if SK has been used between 1 year and 5 days ago
·
Complications: 1% risk of stroke
·
Watch this space for platelet
receptor blocking drugs (eg IIb/IIIa inhibitors)
o Consider for primary angioplasty (acute stenting of an occluded coronary
artery) if large anterior infarct refractory to thrombolysis
·
Management of preload, afterload
and heart rate and rhythm:
o Glyceryl trinitrate
o ACE inhibitor + b-blocker (unless contra-indicated)
o Bed rest
·
Monitor ECG, BP, cardiac enzymes,
ABGs
·
Stop smoking
·
Early stress/treadmill test
Prognosis
·
Good prognostic indicators:
o No pre-existing hypertension
o Normal heart size
o No post MI pulmonary oedema
o No significant arrhythmias after day 1
o No post-MI angina
·
If good prognosis, discharge on
aspirin and b-blocker. Add an ACE inhibitor if ¯LVF. Consider a statin if lipids.
Complications
·
35% die within one year, 10% per
year thereafter. NZ overall hospital
mortality 19%
·
Arrhythmias and conduction
defects: eg premature ventricular beats, sinus bradycardia, VT, VF, heart block
·
Extension of infarction,
re-infarction
·
Congestive heart failure
(pulmonary oedema): everyone who‟s had a significant MI will have some degree
of this
·
Cardiogenic shock: if more than
40% of the left ventricle is infarcted.
70 – 90% die
·
Pericarditis: fibrinous adhesions
in the pericardium overlying the infarct (Dressler‟s syndrome – autoimmune
adherent pericarditis – occurring 2 – 6 weeks post MI or cardiac surgery.
Treatment - steroids)
·
Mural thrombosis ®
embolisation
·
Myocardial rupture ®
tamponade. Maximum incidence day 5 - 7. Can include rupture of interventricular
septum
·
Papillary muscle rupture or
infarct ® mitral incompetence
·
Ventricular aneurysm formation:
12 – 20% of cases
·
Ischaemic cardiomyopathy: severe
atherosclerosis involving all major branches ® inadequate
vascular supply ® myocyte loss and interstitial fibrosis ® ¯compliance
& dilation ® compensation by myocyte hypertrophy ® slow progressive heart failure
and enormous heart size (up to 2 to 3 times normal)
·
Time to complications:
o 1 – 3 days: arrhythmia, CHF, pericarditis
o 5 – 7 days: rupture
o Later: recurrent MI, angina, embolism from mural thrombosis, mitral
regurgitation, Dressler‟s syndrome (Post MI syndrome)
Related Topics