Chapter: Medicine Study Notes : Cardiovascular
Hypertension
Hypertension
· See Measuring Blood Pressure(Topic), for measurement
· Is a risk factor not a disease
· Definition:
o No dividing line between normal and high blood pressure. There are arbitrary levels set based on the risk of complications (the main ones being stroke, MI, heart failure and renal failure)
o In determining whether the blood pressure is „bad‟, take into account the systolic and diastolic pressure, age, sex, other diseases (eg DM, hyperlipidaemia), smoking. Older age is the greatest risk factor: treat high blood pressure in an older person regardless of other risk factors
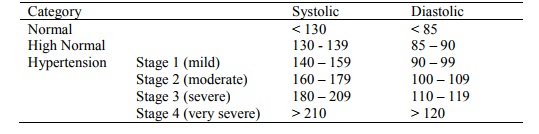
o WHO definitions:
o Also classified according to retinopathy, see Hypertensive Retinopathy(Topic)
· Classified as:
o Primary/essential (what most people have – but a diagnosis of exclusion): contributing factors include hereditary, obesity, alcohol intake, salt intake (60% of patients respond to ¯salt intake – but compliance difficult)
o Secondary causes: renal disease (eg renal artery stenosis, diabetic kidney disease, etc), endocrine (eg cortisol, aldosterone, acromegaly, oral contraceptives), neurogenic (eg psychogenic), sleep apnoea (major changes in baroreceptor reflexes)
· Epidemiology:
o Prevalence with age. Older people at greater risk at any given blood pressure compared with young
o Strong risk factor for stroke, congestive heart failure, coronary artery disease and renal failure
o Probably 10 – 20% of older adults require treatment (ie have essential hypertension with diastolic pressure > 95 mmHg)
o Treatment reduces related complications. Stroke risk reduces in line with BP, MI risk doesn‟t reduce as much for a given drop in BP
· History:
o How accurate is the diagnosis?
o Usually symptomless
o Possibly related symptoms: palpitation, flushing, headache
o Related risk factors: history of renal, cardiac or neurological disease
o Asthma, diabetes, gout, renal disease: complications with drug treatment
o Occupational
o Diet: salt, fat
o Smoking and alcohol
o Family History
· Detection and assessment:
o Blood pressure more labile in older adults Þ measure 2 to 3 times (in same arm). Measure standing and sitting
o In primary hypertension usually on standing. In secondary hypertension, usually ¯ on standing
o Basic workup:
§ Urine for protein, blood and glucose ® DM, renal disease
§ FBC for polycythaemia, renal disease, alcohol
§ Electrolytes (especially K): exclude odd endocrine causes
§ ECG: any end organ damage
o Additional tests if indicated:
§ Microscopic analysis of urine (for casts)
§ Plasma lipids
§ Blood glucose: need to modify drug treatment
§ Serum Ca, PO4, uric acid (gout – associated with hypertension, may also due to drugs)
§ Echocardiogram or CXR
§ Special tests for secondary causes if indicated: eg renal imaging, 24 hour urine for catecholamine metabolites (phaeochromocytoma)
· Pathology:
o Pathophysiology: poorly understood. Older people have ¯renin, and are more responsive to Na depletion. „Hardening‟ of arteries ®systolic pressure. ¯Responsiveness to b-mediated vascular relaxation
o Leads to hypertensive heart disease: left ventricular hypertrophy ® relative myocardial ischaemia. Aortic valvular disease also ® LV hypertrophy
o Malignant hypertension (accelerated hypertension): hypertension leading to rapidly progressive vascular compromise. Blood vessels show fibrinoid necrosis or concentric hyperplasia („onion skin‟ changes)
Non-drug treatment
· Remove/substitute drugs: eg NSAIDs, OCP, Prednisone
· Always attempt lifestyle changes first:
o Stop smoking (little effect on BP, but biggest impact on risk factors)
o Weight loss
o ¯Alcohol (max 2 drinks per day)
o ¯Salt intake (max 70 mmol/day)
o exercise
o ¯Saturated fats
Drug Treatment
· When to treat:
o Given it is such a strong risk factor, consider hypertension above systolic 140 mmHg
o Always treat > 170 systolic or > 110 diastolic
o Hardly ever treat < 140 and < 90 diastolic
o In between, controversial. Consider other risks. If over 65 no other risk factors needed (eg diabetes, etc). Give considerable attention to non-pharmacological approaches for 3 – 6 months. Long term follow up necessary
o Treat 72 older adults for 5 years to prevent 1 death, treat 43 for 5 years to prevent one cerebrovascular event
o Aim of treatment: diastolic < 90
· Rules of thumb:
o Use low doses of several agents, rather than increasing doses of one drug (especially thiazides)
o First line: thiazides (with or without a potassium sparing agent) and/or b-blocker (atenolol most used in trials). If tolerate them both then add them together
o ACE inhibitors: not so effective but rated best quality of life
o Don‟t take diuretic, ACE inhibitor and NSAIDS together (renal side effects)
o Introduce slowly, monitor for symptoms and postural hypotension
o Aim for 140/90, and then attempt back titration 3 monthly
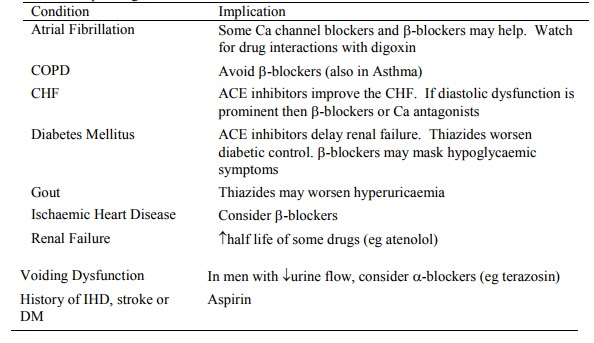
· Individualise depending on co-morbid conditions:
Related Topics