Chapter: Orthopaedics
Pediatric Orthopaedics
Pediatric Orthopaedics
Fractures in Children
·
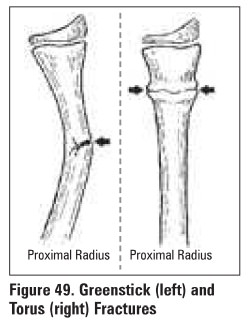
type of fracture
o
usually greenstick or buckle because periosteum is
thicker and stronger
o
adults fracture through both cortices
·
epiphyseal growth plate
o
plate often mistaken for fracture and vice versa
o
x-ray opposite limb for comparison
o
mechanism which causes ligamentous injury in
adults causes growth plate injury in children
o
intra-articular fractures have worse consequences
in children because they usually involve the growth plate
·
anatomic reduction
o
gold standard with adults
o
may cause limb length discrepancy in children
(overgrowth)
o
accept greater angular deformity in clilldren
{remodeling minimizes deformity)
·
time to heal
o
shorter in children
·
always be aware of the possibility of child abuse
o
make sure mechanism compatible with injury
o
high index of suspicion. look for other signs,
including x-ray evidence of healing fractures at other sites
Stress Fractures
Mechanism
·
insufficiency fracture
o
stress applied to a weak or structurally deficient
bone
·
fatigue fracture
o
repetitive. excessive force applied to normal bone
·
most common in adolescent athletes
·
tibia is most common site
Diagnosis and Treatment
·
localized pain and tenderness aver. the involved
bone
·
plain films may not show fracture for 2 weeks
·
bone scan +ve in 12-15 days
·
treatment is rest from strenuous activities to allow
remodeling (can take several months)
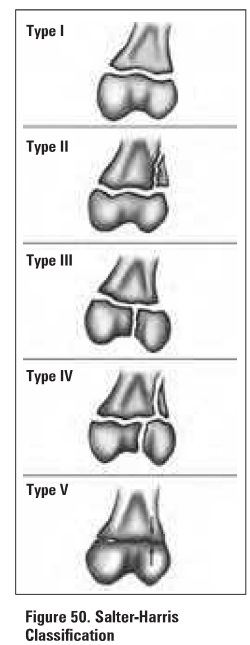
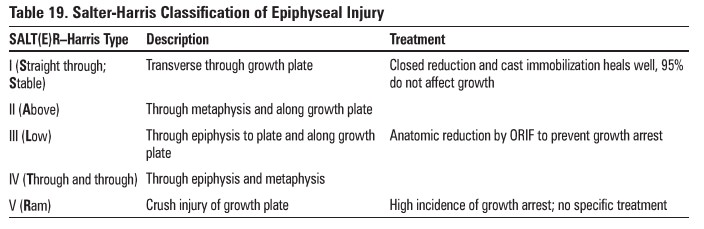
Epiphyseal Injury
Slipped Capital Femoral Epiphysis (SCFE)
·
type I Salter-Harris epiphyseal injury
·
most common adolescent hip disorder, peak at
pubertal growth spurt
·
risk factors: male, obese, hypothyroid
Etiology
·
multifactorial
o
genetic: autosomal dominant, blacks >
caucasians
o
cartilaginous physis thickens rapidly under growth
honnone (GH) effects
o
sex honnone secretion, which stabilizes physis,
has not yet begun
o
overweight: mechanical stress
o
trauma: causes acute slip
Clinical Features
·
acute: sudden, severe pain with limp
·
chronic: limp with medial knee or anterior thigh
pain
·
tender over joint capsule
·
restricted internal rotation, abduction, flexion
Whitman's
sign: with flexion there is an obligate external rotation of the hip
·
pain at extremes of ROM
Investigations
·
x-rays: AP, frog-leg, lateral radiographs
• posterior and medial slip
• if mild slip, AP view may be normal or show
slightly widened growth plate compared with opposite side
Treatment and Complications
·
mild/moderate slip: stabilize physis with pins in
current position
·
severe slip: ORIF or pin physis without reduction and
osteotomy after epiphyseal fusion
·
complications: AVN (most common), chondrolysis,
pin penetration, premature OA, loss of ROM
Developmental Dysplasia of the Hip (DOH)
·
formerly called congenital dysplasia of the hip
(CDH)
·
due to ligamentous laxity, muscular
underdevelopment, and abnormal shallow slope of acetabular roof
·
spectrum of conditions that lead to hip
subluxation and dislocation
o
dislocated femoral head completely out of
acetabulum
o
dislocatable head in socket
o
head subluxates out of joint when provoked
o
dysplastic acetabulum, more shallow and more
vertical than normal
·
painless (if painful suspect septic dislocation)
Physical Examination
·
diagnosis is clinical
o
limited abduction of the flexed hip ( <50-600)
o
affected leg shortening results in asymmetry in
skin folds and gluteal muscles, wide perineum
o
Barlow's test (for dislocatable hip)
o
–flex hips and knees to 90° and grasp thigh
o
–fully adduct hips, push posteriorly to try to dislocate
hips
·
Ortolani's test (for dislocated hip)
o
initial position as above but try to reduce hip
with fingertips during abduction
o
positive test: palpable clunk is felt (not heard)
ifhip is reduced
·
Galeazzi's Sign
o
knees at unequal heights when hips and knees
flexed
o
dislocated hip on side oflower knee
o
difficult test ifchild <1 year
·
false positive if congenital short femur
o
Trendelenburg test and gait useful ifolder (>2
years)
Investigations
·
U/S in first few months to view cartilage
·
follow up radiograph after 3 months
Treatment and Complications
·
0-6 months: reduce hip using Pavlik harness to maintain
abduction and flexion
·
6-18 months: reduction under GA, hip spica cast x
2-3 months (if Pavlik harness fails)
·
>18 months: open reduction; pelvic and/or
femoral osteotomy
·
complications
o
redislocation, inadequate reduction, stiffness
o
AVN of femoral head
Legg-Calva-Perthes Disease (Coxa Plana)
·
self-limited AVN of femoral head. presents at 4-10
years of age
·
etiology unknown, 20% bilateral, males>
females, 1/10,000
·
associations
o
family history
o
low birth weight
o
abnormal pregnancy/delivery
o
history of trauma to affected hip
·
key features
o
AVN of proximal femoral epiphysis, abnormal growth
of the physis, and eventual remodelling of regenerated bone
Clinical Features
·
child with hip pain and limp
·
tender over anterior thigh
·
flexion contracture: decreased internal rotation,
abduction of hip
Investigations
·
x-rays
o
may be negative early
o
eventually, characteristic collapse of femoral
head (diagnostic)
·
subchondral fracture
·
metaphyseal cyst
Treatment
·
goal is to preserve ROM and preserve femoral head
in acetabulum
·
PT: ROM exercises
·
brace in flexion and abduction x 2-3 years
·
femoral or pelvic osteotomy
·
prognosis better in
o
males <5 years old. <50% of femoral head
involved, abduction >30°
·
50% of involved hips do well with conservative
treatment
·
complicated by early onset osteoarthritis and
decreased ROM
Osgood-Schlatter Disease
Mechanism
·
repetitive tensile stress on insertion of patellar
tendon over the tibial tuberosity causes minor avulsion at the site and subsequent
inflammatory reaction (tibial tubercle apophysitis)
·
most common in adolescent athletes, especially
jumping sports
Clinical Features
·
tender lump over tibial tuberosity
·
pain on resisted leg extension
·
anterior knee pain exacerbated by jumping or kneeling,
relieved by rest
Investigations
·
x-rays: fragmentation of the tibial tubercle, ±
ossicles in patellar tendon
Treatment
·
benign, self-limited condition
·
may restrict activities such as basketball or
cycling
·
flexibility, strengthening exercises
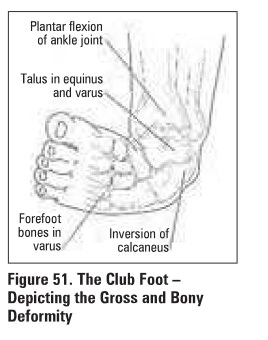
Congenital Talipes Equinovarus (Club Foot)
·
fixed deformity
·
3 partB to defonnity
o
talipes: talus is inverted and internally rotated
o
equinus: ankle is plantar flexed
o
varus: heel and forefoot are in varus (supinated)
·
may be idiopathic, neurogenic, or syndrome-associated
·
1-2/1,000 newborns, 50% bilateral, occurrence
M>P, severity P>M
Physical Examination
·
examine hips fur associated DDH
·
examine knees for deformity
·
examine back for dysrapbiam (unfused vertebral
bodies)
Treatment
·
correct deformities in the following order
(Ponseti Technique):
o
furefoot adduction, ankle inversion, equinus
o
–––change strapping/C81it ql-2 weeks
·
surgical release in refractory case (50%)
o
–––delayed until 3-4 months of age
·
3 year recurrence rate = S-10%
·
mild recurrence common; affected foot is
permanently smaller/stiffer than normal foot with calf muscle atrophy
Scoliosis
Definition
·
lateral curvature of spine with vertebral rotation
Epidemiology
·
age: 10-14 years
·
more frequent and more severe in females
Etiology
·
idiopathic: most common (90%)
·
congenital: vertebrae fail to form or segment
·
neuromuscular: UMN or LMN lesion, myopathy
·
other: osteochondrodystrophies, neoplastic,
traumatic
·
portural: leg length discrepancy, muscle spum
Clinical Features
·
± back. pain
·
1° where several vertebrae affected
·
2° above and below fixed 1o to try and maintain
normal position of head and pelvis
·
asymmetric shoulder height when bent forward
·
• Adam's test: rib hump when bent forward
·
prominent scapulae, creased flank, asymmetric
pelvis
·
aaaociated posterior midline skin lesions in
non-idiopathic scolioses
o
cafe-au-lait spots, dimples, neuro1ibromas
o
axillary freckling. hemangiomas, hair patches
·
associated pes cavus or leg atrophy
·
apparent leg length discrepancy
X-Raya
·
3-foot standing
·
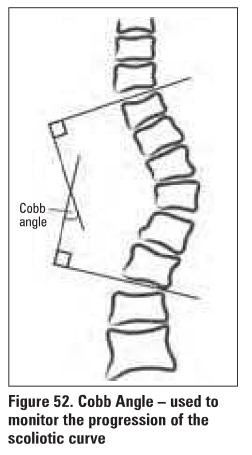
measure curvature - Cobb Angle (Figure 52)
·
may have associated kyphoala
Treatment
·
based on degree of curvature
o
<20°: observe for changes
o
>20° or progressive: bracing (many types) that
halt/slow curve progression but do NOT reverse deformity
o
>40°, cosmetically unacceptable or respiratory
problems: surgical correction (spinal fusion)
Related Topics