Chapter: Orthopaedics
Fractures - General Principles
Fractures - General
Principles
Fracture Description
1. Integrity of Skin/Soft Tissue
·
closed: skin/soft tissue over and near fracture is
intact
·
open: akin/soft tissue over and near fracture is
lacerated or abraded, fracture exposed to outside environment. continuous
bleeding from puncture sl1e or fat droplets in blood suggest communication with
fracture
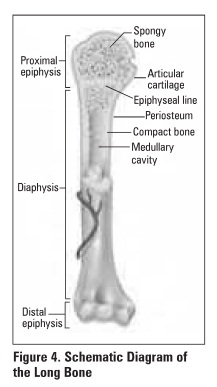
2. Location (Figure 4)
·
epiphyseal: end of bone, forming part of the adjacent
joint
·
metaphyseal: the flared portion of the bone at the
ends of the shaft.
·
diaphyseal: the shaft of a long bone (proximal,
middle, distal)
·
physis: growth plate
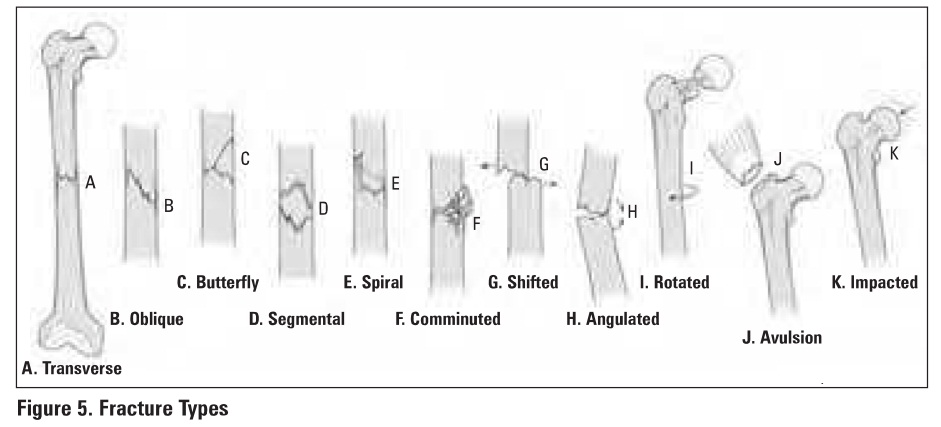
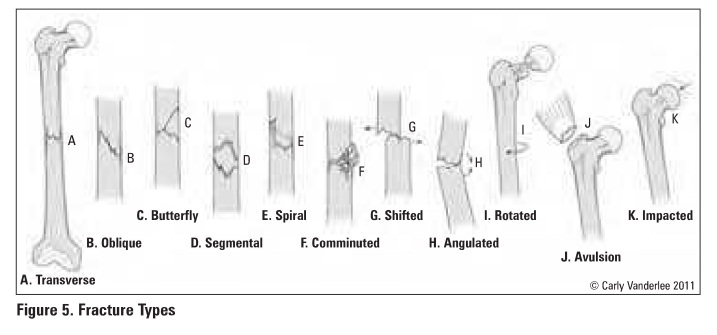
3. Orientation/Fracture Pattern (Figure 5)
·
transverse: perpendicular fracture line, direct
force, high energy
·
oblique: angular fracture line, angular or
rotational force
·
butterfly: slight comminution at the fracture site
which looks like a butterfly
·
segmental: a separate segment of bone bordered by
fracture lines, high energy
·
spiral: complex, multi-planar fracture line,
rotational force, low energy
·
comminuted/multl-fragmenary: more than 2 fracture
fragments
·
intra-articular: fracture line crosses artlcu1ar
cartilage and enters joint
·
compression/Impacted: impaction of bone, e.g.
vertebrae, proximal. tibia
·
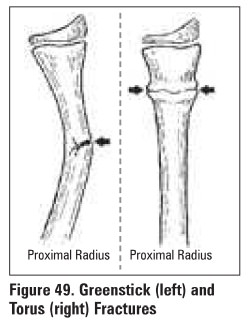
torus: a buckle fracture of one cortex. often in
children (Figure 49)
·
green-stick: an incomplete fracture of one cortex,
often in children (Figure 49)
·
pathologic: fracture through bone wakened by
disease/tumour
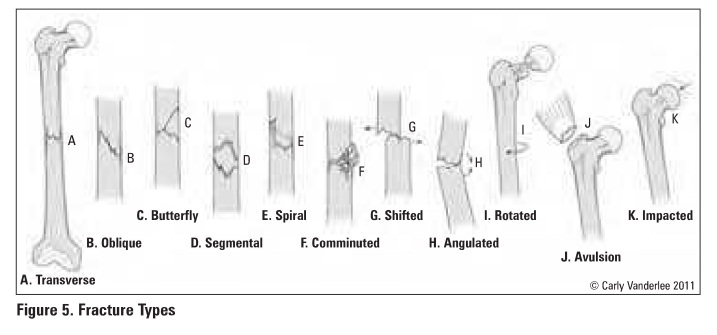
4. Displacement (Figure 5)
·
nondisplaced: fracture fragments are in anatomic
alignment
·
displaced: fracture fragments are not in anatomic
alignment
·
distracted: fracture fragments are separated by a
gap
·
angulated: direction of fracture apex. e.g.
varus/valgus
·
translated: percentage of overlapping bone at
fracture site
·
rotated: fracture fragment rotated about long axis
of bone
Management of Fractures
·
ABCs, primary survey and secondary survey (ATLS
protocol)
o
rule out other fractures/injuries
o
rule out open fracture
·
AMPLE history - Allergies, Medications, Past
medical history, Last meal, Events surrounding injury
o
consider pathologic fracture with history of only
minor trauma
·
additional history/physical:
o
baseline functional status -handedness (upper
extremity) vs. ambulatory ability (lower ertremity- note distances, stairs, and
use of assistive devices such as canes, walkers, wheelchairs, etc.)
o
occupation and smoking status
o
mechanism of injury
o
past medical history (note any contraindications to
or general anesthetic)
o
neurovascular status
·
analgesia
·
imaging
·
splint extremity
1. obtain
the .reduction (refer to Table 22 for appropriate IV sedation)
·
closed reduction
•
apply traction in the long am of the limb
•
reverse the mechanism that produced the fracture
•
reduce with IV sedation and muscle relaxation
(fluoroscopy can be used if available)
·
indications for open reduction - NO CAST
·
other indications include
•
failed closed reduction
•
cannot cast or apply traction due to site (e.g.
hip fracture)
•
pathologic fractures
•
potential fur improved function with open
reduction and Internal fiDtion (ORIF)
·
potential complications of open reductions
•
infection
•
mal-union
•
non-union
•
implant failure
•
new fracture
·
re-check. neurovascular status after .reduction
and obtain post-reduction x-ray
2.
maintain the reduction
·
external stabilization - splints, casts, traction,
external fixator
·
internal stabilization -percutaneous pinning, extra
rnedullary fixation (screws, plates, wires), intramedullary fixation (rods)
·
follow-up- evaluate bone healing
3.
rehabilitate to regain function and
avoid joint stiffness

Fracture Healing
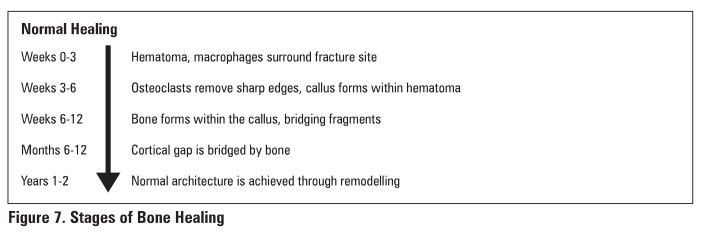
Evaluation of Healing: Testa of Union
·
clinical.: No longer tender to palpation or stressing
on physical exam
·
x-ray: trabeculae cross fracture site. visible
callus bridging site on at least 3 of 4 cortices
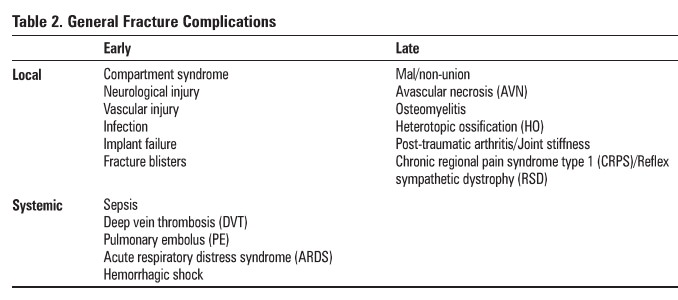
General Fracture Complications
Table 2.
General Fracture Complications
Related Topics