Chapter: Orthopaedics
Orthopaedics: Spine
Spine
Fractures of the Spine
·
see Neurosurgery
·
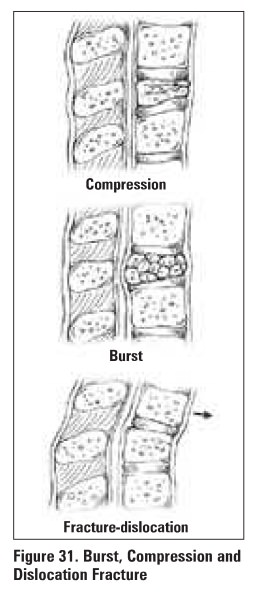
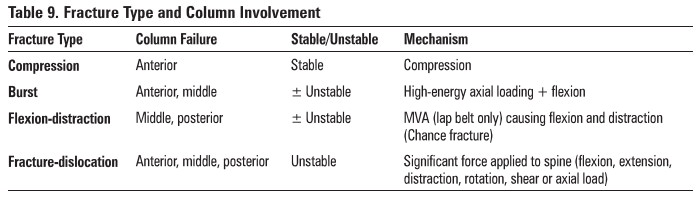
4 main types of :fractures (see Table 9)
Table 9. Fracture Type and Column involvement
Cervical Spine
General Principles
·
Cl = atlas: no vertebral body, no spinous process
·
C2 = axis: odontoid= dens
·
7 cervical vertebrae; 8 cervical nerve roots
·
nerve root exits above vertebra (Le. C4 nerve root
exits above C4 vertebra)
·
radiculopathy = Impingement of nerve root
·
myelopathy = Impingement of spinal cord
Special Testing
·
Compression test pressure on head worsens radicular
pain
·
Diattaction test: traction on head relieves
radicular symptoms
·
Valsalva test: Valsalva maneuver increase intrathecal
pressure and causes radicular pain
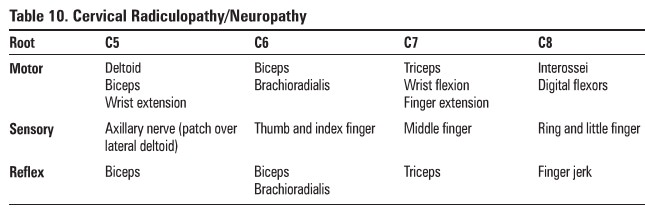
Table 10. Cervical Radiculopathy/Neuropathy
X-Rays for C-Spine
·
AP spine: alignment
·
AP odontoid: atlantoaxial articulation
·
lateral
o
vertebral alignment: posterior vertebral bodies
should be aligned (translation >3.5 mm is abnormal)
o
angulation: between adjacent vertebral bodies
(> 11 • is abnormal)
o
disc or facet joint widening
o
anterior soft tissue space (at C3 should be =<3
mm; at C4 should be =<8-10 mm)
·
oblique: evaluate pedicles and intervertebral
foramen
·
± swimmer's view: lateral view with arm abducted
1800 to evaluate C7-T1 junction if lateral view is inadequate (must see C7-T1
in all trauma situations)
·
± lateral flexion/extension view: evaluate
subluxation of cervical vertebrae
Differential Diagnosis of C-Spine Pain
·
trapezial sprain, whiplash, cervical spondylosis,
cervical stenosis, rheumatoid arthritis (spondylitis), traumatic injury
Thoracolumbar Spine
General Principles
·
spinal cord terminates at conus medullaris (Ll)
·
individual nerve roots exit below pedicle of
vertebra (ie. LA nerve root exits below LA pedicle)
Special Tests
·
Straight leg raise (SLR): passive lifting of leg
(30-70°) reproduces radicular symptoms of pain radiating down post/lat leg to knee,
± into foot
·
Lasegue maneuver: dorsiflexion offoot during SLR
makes symptoms worse or, if leg is less elevated, dorsiflexion will bring on
symptoms
·
Femoral stretch test: with patient prone, flexing
the knee of the affected side and passively extending the hip results in
radicular pain
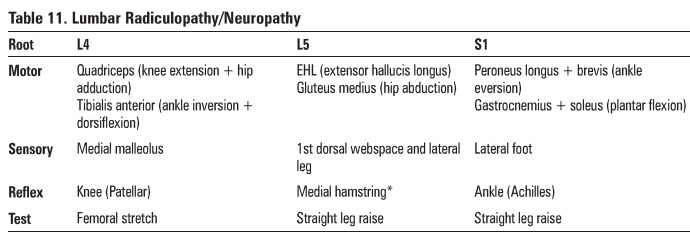
Table 11.
Lumber Radiculopathy/Neuropatlly
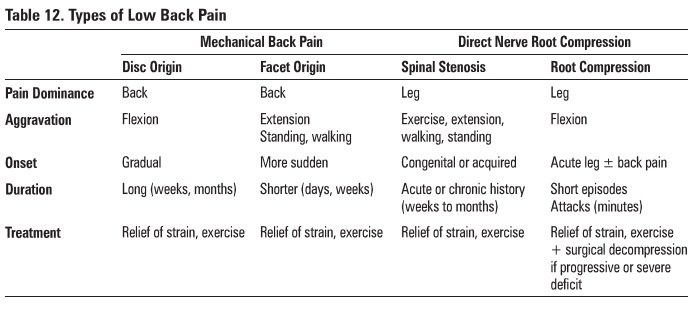
Diffarantial Diagnosis af Bilek Pain
1 .
mechanical or nerve compression (>90%)
·
degenerative (disc, facet, ligament)
·
peripheral nerve compression (disc herniation)
·
spinal stenosis (congenital. osteophyte, central
disc)
·
cauda equJna syndrome
2.others
·
neoplastic (primary. metastatic, multiple myeloma)
·
infectious (osteomyelitis, TB)
·
metabolic (osteoporosis)
·
traumatic fracture (compression, distraction,
translation, rotation)
·
spondyloarthropathies (ankylosing spondylitis)
·
referred (aorta, renal, ureter, pancreas)
DEGENERATIVE DISC DISEASE
·
loss of vertebral disc height with age results in:
o
bulging and tears of annulus fibrosus
o
change in alignment of facet joints
o
osteophyte formation
·
can cause back-dominant pain
·
management
o
non-operative
o
––staying active with modified activity
o
––back strengthening
o
––NSAIDs
o
––do not treat with opioids; no proven efficacy of
spinal traction or manipulation
·
operative - rarely indicated
o
decompression ± fusion
o
no difference in outcome between non-operative and
surgical management at 2 years
SPINAL STENOSIS
·
definition: narrowing of spinal canal <10 mm
·
etiology: congenital (idiopathic, osteopetrosis,
achondroplaai.a) or acquired (degenerative, iatrogenic- post spinal surgery,
ankylosmg spondylosis, Paget's disease, trauma)
·
clinical features
o
± bilateral back and leg pain
o
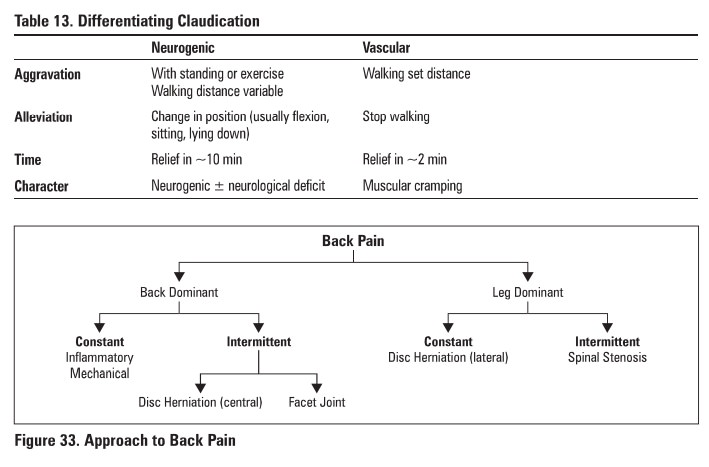
neurogenic claudication (see Table 13)
o
± motor weakness
o
normal back flexion; difficulty with back
extension
·
investigations: cr1MRI reveals narrowing of spinal
canal, but gold standard = CT myelogram
·
treatment
o
non-operative: vigorous PT (flexion exercises,
stretch/strength exmises), NSAIDs, lumbar epidural. steroids
o
operative: decompression surgery if conservative
methods failed >6 months
MECHANICAL BACK PAIN
·
definition: back pain NOT due to prolapsed disc or
any other clearly defined pathology
·
clinical features
o
dull backache aggravated by activity
o
morning stiffness
o
no neurological signs
·
treatment: symptomatic (analgesics, PT)
·
prognosis: symptoms may resolve in 4-6 weeks,
others become chronic
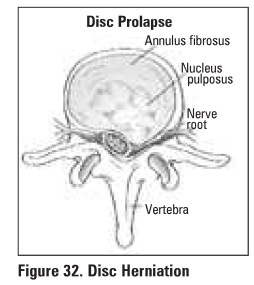
LUMBAR DISC HERNIATION
·
definition: tear in annulus fibrosus allows
protrusion of nucleus pulposus causing either a central, posterolateral or
lateral disc herniation, most commonly at LS-Sl > 14-5 > L3-4
·
etiology: usually a history of flexion-type injury
which tears the annulus fibrosus allowing for protrusion of the nucleus
pulposus
·
clinical features
o
–back dominant pain (central herniation) or leg
dominant pain (lateral herniation)
o
–tenderness between spines at affected level
o
–muscle spasm ± loss of normal lumbar lordosis
o
–neurological disturbance is segmental and varies
with level of central herniation
o
–––motor weakness (L4, LS, Sl)
o
–––diminished reflexes (14, Sl)
o
–––diminished sensation (L4, 15, Sl)
o
+ve straight leg raise
o
+ve Lasegue test
o
bowel or bladder symptoms, decreased rectal tone
suggests cauda equina syndrome due to central disc hernation - surgical
emergency
·
investigations: MRI
·
treatment
o
symptomatic
o
–extension protocol (PT)
o
–NSAIDs
o
–90% resolve in 3 months
o
surgical discectomy reserved for progressive
neurological deficit, failure of symptoms to resolve within 3 months or cauda
equina syndrome due to central disc herniation
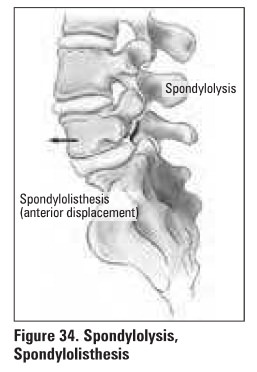
SPONDYLOLYSIS
·
definition: defect in the pars interarticularis
with no movement of the vertebral bodies
·
etiology
o
trauma: gymnasts, weightlifters, backpackers,
loggers, labourers
·
clinical features: activity-related back pain
·
investigations
o
oblique x-ray: "collar" break in the
"Scottie dog's" neck
o
bone scan
o
CT scan
·
treatment: activity restriction, brace, stretching
exercise
SPONDYLOLISTHESIS
·
definition: defect in pars interarticularis
causing a forward slip of one vertebrae on another usually at LS-Sl, less
commonly at L4-5
·
etiology: congenital (children), degenerative
(adults), traumatic, pathological, teratogenic
·
clinical features: lower back pain radiating to buttocks
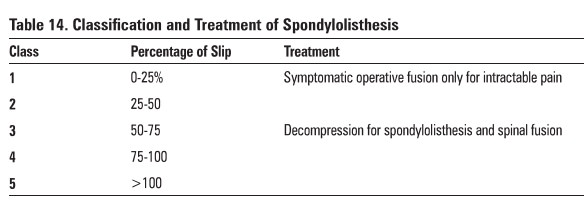
Table 14. Classification and Treatment of Spondylolisthesis
Class:
Percentage of Slip & Treatment
0-25% Symptomatic operative fusion only for
intractable pain
25-50
50-75 Decompression for spondylolisthesis and
spinal fusion
75-100
>100
Specific Complications
·
may present as cauda equina syndrome due to roots
being stretched over the edge of LS or sacrum
Related Topics