Chapter: Orthopaedics
Orthopaedics: Wrist
Wrist
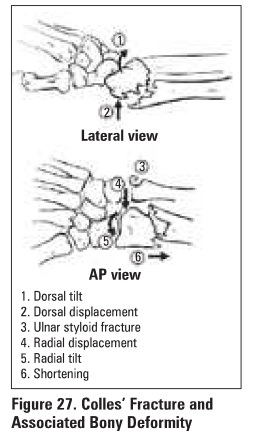
Colles' Fracture
Definition
·
transverse distal radius fracture (about 2 an
proximal to the radiocarpal Joint) with dorsal displacement ± ulnar styloid
fracture
Epidemiology
·
most common fracture in those >40 years,
espedal1y in women and those with osteoporotic bone
Mechanism
·
FOOSH
Clinical Features
·
dinner fork'" deformity
·
swelling, ecchymosis, tenderness
Investigations
·
findings on x-ray (Figure 27)
Treatment
·
goal is to restore radial height, radial
inclination (22•), volar tilt (11 °) and articular congruity
·
closed reduction (think. opposite of the
deformity):
o
hematoma block (sterile prep and drape, local
anesthetic injection directly into fracture site) or conscious sedation
o
closed reduction -traction with extension
(exaggerate injury), then traction with ulnar deviation, pronation, flexion of
distal fragment - not at wrist)
·
dorsal slab/below elbow cast for 5-6 weeks
·
x-ray ql week to ensure reduction is maintained
·
obtain post-reduction films immediately; repeat
reduction if necessary, consider external fixation or ORIF
Smith's Fracture
Definition
·
volar displacement of the distal radius (i.e.
reverse Colles' fracture)
Mechanism
·
fall onto the back of the flexed hand
Treatment
·
usually unstable and needs ORIF
·
if patient is poor operative candidate, may
attempt non-operative treatment
·
closed reduction with hematoma block (reduction
opposite of Colles')
·
long-arm cast in supination x 6 weeks
Complications of Wrist Fractures
·
most common complications are poor grip strength,
stiffness, and radial shortening
·
distal radius fractures in individuals <40
years of age are usually highly comminuted and are likely to require ORIF
·
80% have normal function in 6-12 months
·
early
o
difficult reduction ± loss of reduction
o
compartment syndrome
o
extensor pollicis longus (EPL) tendon rupture
o
acute carpal tunnel syndrome
o
finger swelling with venous or lymphatic block
·
late
o
mal-union, radial shortening
o
painful wrist secondary to ulnar prominence
o
frozen shoulder ("shoulder-hand syndrome'')
o
post-traumatic arthritis
o
carpal tunnel syndrome
o
complex regional pain syndrome (reflex sympathetic
dystrophy (RSD))
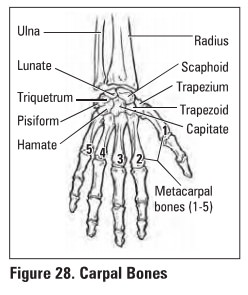
Scaphoid Fracture
Epidemiology
·
common in young men; not common in children or in
patients beyond middle age
Mechanism
·
FOOSH resulting most commonly in a transverse
fracture through the waist (middle) of the scaphoid

Clinical Features
·
pain on wrist movement
·
tenderness in scaphoid region (anatomical
"snuff box")
·
usually undisplaced
Investigations
·
x-ray: AP, lateral, scaphoid views with wrist
extension and ulnar deviation q2 weeks
·
±bone scan
·
±CT,MRI
·
Note: a fracture may not be radiologically evident
up to 2 weeks after acute injury, so if a patient complains of wrist pain and
has anatomical snuffbox tenderness but a negative x-ray, treat as if positive
for a scaphoid fracture and repeat x-ray 2 weeks later to rule out a fracture.
If x-ray still negative order CT or MRI
Treatment
·
non-displaced= long-arm thumb spica cast x 4 weeks
then short arm cast until radiographic evidence of healing is seen (2-3 months)
·
displaced = open (or percutaneous) screw fixation
Specific Complications (see
General Fracture Complications)
·
AVN of the proximal fragment (since the scaphoid
has distal to proximal blood supply, the more proximal the fracture, the
greater incidence of AVN)
·
delayed union (recommend surgical fixation)
·
non-union (must use bone graft and fixation to heal)
Prognosis
·
fractures of the proximal third of the scaphoid
have 70% rate ofnon-union or AVN
·
waist fractures have healing rates of 80-90%
·
distal third fractures have healing rates close to
100%
Related Topics