Chapter: Orthopaedics
Orthopaedic Emergencies
Orthopaedic Emergencies
Trauma Patient Work-Up
Etiology
·
high energy trauma e.g. motor vehicle accidents,
fall from height
·
may be associated with spinal injuries or
life-threatening visceral injuries
Clinical Presentation
·
local swelling, tenderness, deformity of the limbs
and instability of the pelvis or spine
·
decreased level of consciousness
·
consider involvement of alcohol or other
substances
Investigations
·
trauma survey (see Emergency Medicine. Initial
Patient Assessment/Management, ER2)
·
x-rays: !at cervical spine, AP chest, abdo x-ray,
AP pelvis, AP and lateral of all long bones suspected to be injured
·
other views of pelvis: AP, inlet and outlet; Judet
view for acetabular fracture (see Table 15 for classification of pelvic
fractures)
Treatment
·
ABC DEs and initiate resuscitation to life
threatening injuries
·
assess genitourinary injury (rectal exam/vaginal
exam mandatory)
·
external or internal fixation of all fractures
·
DVT prophylaxis
Complications
·
hemorrhage -life threatening (may produce signs and
symptoms of hypovolemic shock)
·
acute respiratory distress syndrome (ARDS)
·
fat embolism syndrome
·
venous thrombosis - DVT and PE
·
bladder/bowel injury
·
neurological damage
·
possible obstetrical difficulties in future
·
persistent sacro-iliac joint pain
·
persistent pain/stiffness/limp/weakness in
affected extremities
·
post-traumatic arthritis ofjoints with
intra-articular fractures
·
sepsis if missed open fracture
Open Fractures
Definition
• fractured bone in communication with the
external environment
Emergency Measures
·
removal of obvious foreign material
·
irrigate with normal saline
·
cover wound with sterile dressings
·
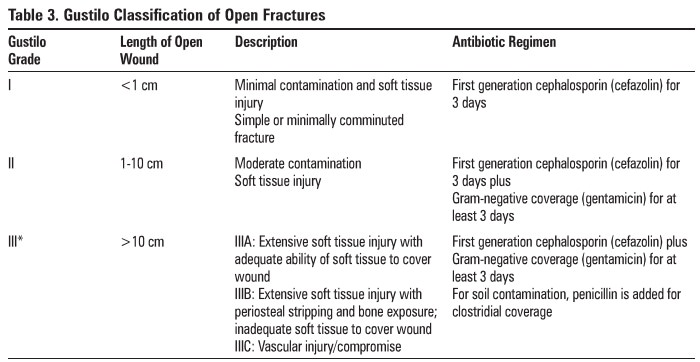
IV antibiotics (see Table 3)
·
tetanus status ± booster
·
splint fracture
·
NPo and prepare for OR (bloodwork, consent, ECG,
CXR)
•
operative irrigation and debridement within 6-8
hours to decrease risk of infection
•
traumatic wound often left open to drain but vac
dressing may be used
•
re-examine with repeat I&D in 48 hrs
Teble 3. Gustilo Classification of Open
Fractures
Septic Joint
Etiology
·
most commonly caused by Staphylococcus aureus in
adults
·
consider coagulase-negative staph in patients with
prior joint replacement
·
consider Neisseria gonorrhoeae in sexually active
adults
·
most common route of infection is hematogenous
Clinical Presentation
·
inability/refusal to bear weight, localized joint
pain, erythema, warmth, swelling with pain on active and passive ROM, ± fever
Investigations
·
x-ray (to r/o fracture, tumour, metabolic bone
disease), ESR, CRP, WBC, blood cultures
·
joint aspirate (WBC >80,000 with >90%
neutrophils, protein level >4.4 mg/dL, joint« blood glucose level, No crystals,
positive Gram stain results)
·
rule out heart murmurs
Treatment
·
IV antibiotics, empiric therapy (based on age and
risk factors), adjust pending joint aspirate C&S
·
for small joints: needle aspiration, serial if
necessary until sterile
·
for major joints such as knee, hip, or shoulder:
urgent decompression and surgical drainage
Osteomyelitis
Etiology
·
most common organism is Staphylococcus aureus
·
consider Salmonella typhi in patients with sickle
cell disease
·
neonates and immunocompromised patients are
susceptible to Gram-negative organisms
·
hematogenous (bacteremia) or exogenous (open
fractures, surgery, local infected tissue) spread
Clinical Presentation
·
localized extremity pain ± fever or swelling 1 to
2 weeks after respiratory infection or infection at another non-bony site
Investigations
·
blood culture, aspirate cultures, ESR, CRP, CBC
(leukocytosis)
·
x-ray, bone scan (increased uptake within 24-48
hours after onset in majority of patients), MRI most sensitive/specific
Treatment
·
IV antibiotics, empiric therapy, adjust pending
blood and aspirate cultures
·
surgical decortication and drainage± local
antibiotics (e_g. antibiotic heads) ifMRI suggests an abscess or if patient
does not improve after 36 hours on IV antibiotics
·
serial I&D (if required), IV antibiotics
eventually changed to PO, splint limb for several weeks followed by protective
weight-bearing of the limb
Compartment Syndrome
Definition
·
increased interstitial pressure in an anatomical
"compartment" (forearm. calf) where muscle and tissue are bounded by
fascia and bone (fibro-osseous compartment) with little room for expansion
·
interstitial pressure exceeds capillary perfusion
pressure leading to muscle necrosis (in 4-6 hrs) and eventually nerve necrosis
Etiology
• intracompartmental: fracture (particularly
tibial shaft fractures, pediatric supracondylar fractures, and forearm
fractures}, crush injury, revascularization
• extracompartmental: constrictive dressing
(circumferential cast), circumferential bum
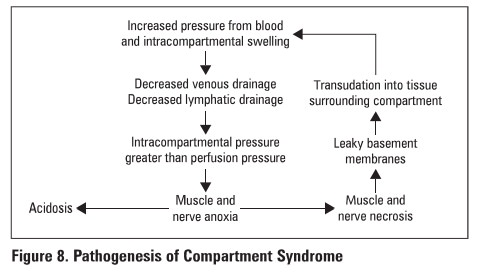
Figure 8. Pathogenesis of Compartment
Syndrome
Physical Examination
·
pain with passive stretch
·
5 P's: late sign
Clinical Features
·
pain with active contraction of compartment
·
pain with passive stretch
·
swollen, tense compartment
·
suspicious history
Investigations
·
usually not necessary as compartment syndrome is a
clinical diagnosis
·
in children or unconscious patients where clinical
exam is unreliable, compartment pressure monitoring with catheter AFTER
clinical diagnosis is made (normal = 0 mmHg; elevated 0!:30 mmHg or S30 mmHg of
diastolic BP)
Treatment
·
non-operative
o
remove constrictive dressings (casts, splints},
elevate limb at the level of the heart
·
operative
o
urgent fasciotomy
o
48-72 hours post-op: wound closure ±necrotic
tissue debridement
Specific Complications
·
rhabdomyolysis, renal failure secondary to myoglobinuria
·
Volkmann's ischemic contracture: ischemic necrosis
of muscle, followed by secondary fibrosis and finally calcification; especially
following supracondylar fracture of humerus
Cauda Equina Syndrome
• see Neurosurgery.
Hip Dislocation
·
full trauma survey
·
examine for neurovascular injury PRIOR to open or
clo&ed reduction
·
reduce hip dislocations ASAP (ideally within 6 hours)
to decrease risk of AVN of the femoral head
·
hip precautions (No extreme hlp flexion,
adduction, internal or external rotation) for 6 weeks post-reduction
·
also see Hip Dislocation after THA
ANTERIOR HIP DISLOCATION
·
mechaniam: posteriorly directed blow to knee with
hlp widely abducted
·
clinical features: shortened, abducted. externally
rotated limb
·
treatment
o
clo3ed reduction under conscious sedation/GA
o
post -reduction CT to assess joint congruity
POSTERIOR HIP DISLOCAT10N
·
most frequent type of hip dislocation
·
mechanism: severe force to knee with hip flexed
and adducted
o
e.g. knee into dashboard in motor vehicle accident
(MVA)
·
clinical features: shortened, adducted and
internally rotated U:mb
·
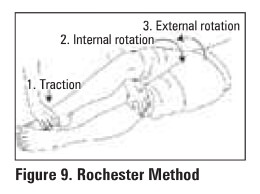
treatment
o
closed reduction under conscious sedation/GA only
if associated femoral neck fracture
o
ORIF if unstable, intra-articular fragments or
posterior wall fracture
o
post-reduction CT to assess joint congruity and
fractures
o
if reduction is unstable, put in traction x 4-6
weeks
CENTRAL HIP DISLOCATION (rare)
·
traumatic injury where femoral head la pushed
through acetabulum toward pelvic cavity
COMPUCAT10NS FOR ALL HIP DISLOCAT10NS
·
post-traumatic arthritis
·
AVN
·
fracture of femoral head. neck. or shaft
·
sciatic nerve palsy in 25% (10% permanent)
·
heterotopic osslfication (HO)
·
thromboembolism- DVT/PE
Related Topics