Chapter: Orthopaedics
Orthopaedics: Shoulder
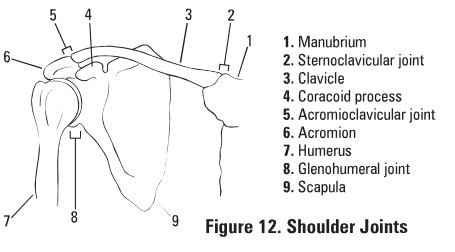
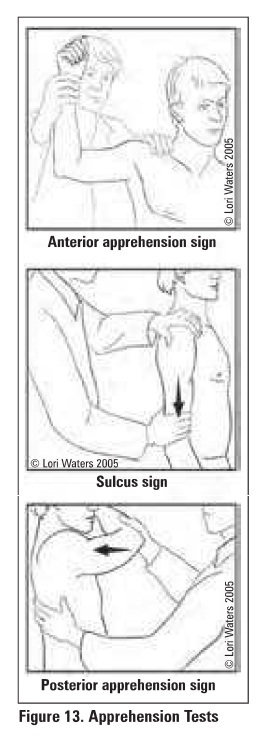
Shoulder
Shoulder Dislocation
·
the glenohumeral joint is the most commonly
dislocated joint in the body since stability is sacrificed for motion
Prognosis
·
recurrence rate depends on age of 1st dislocation:
<20 yrs = 65-95%; 20-40 yrs = 60-70%; >40 yrs = 2-4%
Specific Complications
·
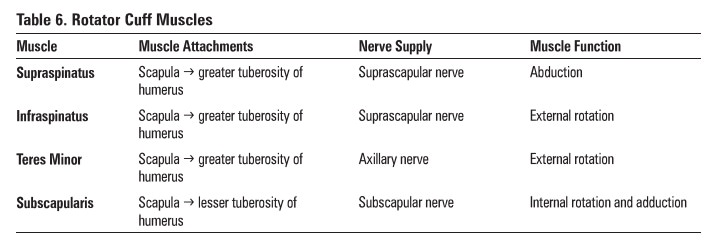
tuberosity fracture, glenoid rim fracture (Bankart
lesion), humeral head impaction (Hill-Sachs lesion)
·
rotator cuff or capsular tear, shoulder stiffness
·
injury to axillary nerve/artery, brachial plexus
·
recurrent/unreduced dislocation (most common
complication)
ANTERIOR SHOULDER DISLOCATION (>90%)
Mechanism
• abducted and externally rotated arm or blow to
posterior shoulder
Clinical Features
·
pain
·
arm held in slight abduction, external rotation;
internal rotation is blocked
·
"squared off" shoulder
·
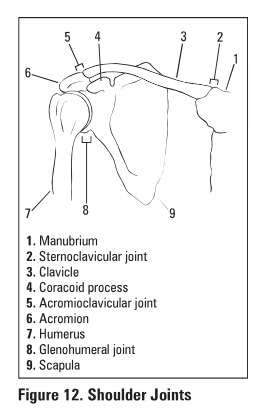
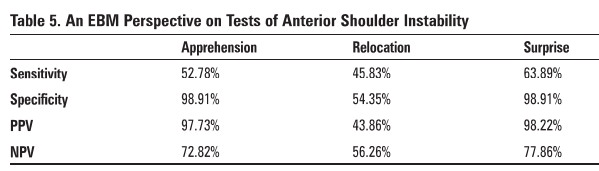
+ve apprehension test: apprehension with shoulder
abduction and external rotation to 90° since humeral head is pushed anteriorly
and recreates feeling of anterior dislocation
·
+ve relocation test: a posteriorly directed force applied
during the apprehension test relieves apprehension since anterior subluxation
is prevented
·
+ve sulcus sign: presence of subacromial
indentation with distal traction on humerus indicates Inferior shoulder
instability
·
neurovascular exam including:
o
axillary nerve (sensory patch over deltoid and
deltoid contraction)
o
musculocutaneous nerve (sensory patch on lateral
forearm and biceps coutraction)
Investigations
• x-rays: AP, trans-sapular, axillary
X-Ray Findings
·
dislocation
o
axillary view: humeral head is anterior
o
trans-scapular view: humeral head is anterior to the
centre of the "Mercedes-Benz sign"
·
± Hill-Sachs lesion: divot in posterior humeral
head due to forceful impaction of an anteriorly dislocated humeral head against
the glenoid rim {Figure 15)
·
±bony Banbart lesion: avulsion of the anterior
glenoid labrum (with attached bone from the glenoid rim
Treatment
·
closed reduction with IV sedation and muscle
rel.uation
·
2methods
o
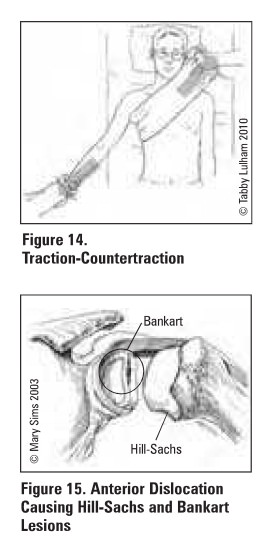
traction-countertraction: assistant stabilizes torso
with a folded sheet wrapped across the chest: while the MD applies gentle
steady traction (see Figure 14)
o
Stimson: while patient lies prone with arm hanging
over table edge, hang a 5lb weight on wrist fur 15-20 min
·
obtain post-reduction .x-rays
·
check post-reduction neurovascular status (NVS)
·
sling x 3 weeks, followed by shoulder
rehabilitation
POSTERIOR SHOULDER DISLOCATION (5%}
·
up to 60-8096 are missed on initial presentation
due to poor physical cum and radiographs
Mechanism
·
adducted, Internally rotated, flexed arm
·
fall on an outstretched hand (FOOSH)
·
3 E's (epileptic seizure, EtOH, electrocution)
·
blow to 81112rior shoulder
Clinical Features
·
arm is held in adduction and internal rotation;
external rotation is blocked
·
anterior shoulder flattening, prominent coracoid,
palpable mass posterior to shoulder
·
posterior apprehension ("jerk") test
with patient supine, 8eJ: elbow and adduct, internally rotate the arm while
applying a posterior force to the shoulder; patient will "jerk"' back
with the sensation of subluxation
Investigation
·
x-rays: AP, trans-scapular, axillary
X-Ray Findings
·
dislocation
o
AP view: partial vacancy of glenoid fosaa (vacant
glenoid sJgn) and >6 mm space between anterior glenoid rim and humeral head
(positive rim sign), humeral head may resemble a lightbulb due to internal
rotation (lightbulb sign)
o
axillary view: humeral head is posterior
o
trans-scapular view: humeral head is posterior to centre
of"Mercedes-Benz signo
·
reverse Hill-Sachs lesion (7596 of cases): divot
in anterior humeral head
·
reverse bony Bankart lesion: avulsion of the posterior
glenoid labrum from the bony glenoid rim
Treatment
·
closed reduction: inferior traction on a flexed
elbow with pressure on the back of the humeral head
·
obtain post-reduction x-rays
·
check post-reduction neurovascular status
·
sling 3 weeks, followed by shoulder rehabilitation
Rotator Cuff Disease
·
rotator cuff consists of 4 muscles that act to
stabilize humeral head within the glenoid
fossa
SPECTRUM OF DISEASE: IMPINGEMENT. TENDONITIS, MICRO OR MACRO TEARS
Etiology
·
compression of rotator cuff tendons (primarily
supraspinatus) and subacromial bursa between the head of the humerus and the
acromion; leads to bursitis. tendonitis and. If left untreated. can lead to rotator
cuff thinning and tear
·
anything that leads to a narrow subacromial space
1. glenohumeral muscle weakness leading to abnormal
motion ofhumeral head
2. scapular muscle weakness leading to abnormal
motion of acromion
3. acromial abnormalities such as congenital
narrow space or osteophyte formation
Clinical Features
·
night pain and difficulty sleeping on affected
side
·
pain worse with active motion
·
weakness and loss of range of motion (e.g. trouble
with overhead activities)
·
tenderness to palpation over greater tuberosity
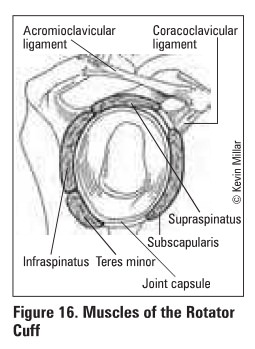
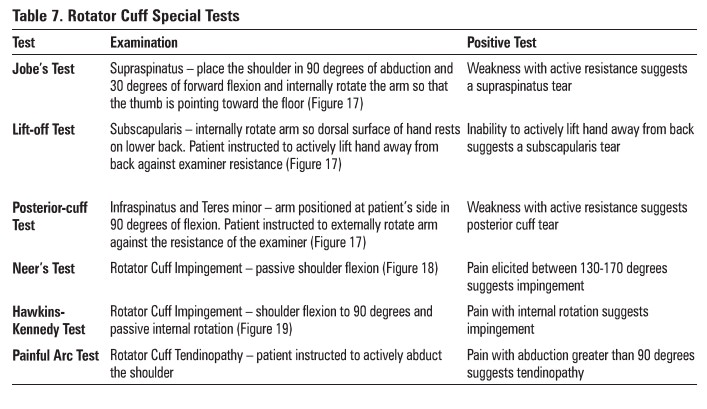
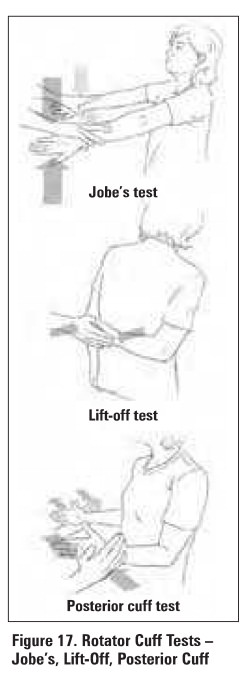
Table 7.
Rotator Cuff Special Tests
lnvestigations
·
X-rays: AP view may show high riding humerus
relative to glenoid, evidence of chronic tendonitis
·
MRI: coronal/sagittal oblique and axial
orientati.Oil8 are useful for assessing full/partial tears and tendinopathy, ±
arthrogram: geyser sign (injected dye leaks out ofjoint through rotator cuff
tear)
·
arthrogram: see full thickness tear, difficult to assess
partial thickness tears
Treatment and Prognoais
·
mild ("wear")
o
treatment is non-operative (physiotherapy, NSAIDs)
·
moderate ("tear")
o
non-operative treatment± steroid Injection
·
severe ("repair")
o
impingement that is refractory to 2-3 months physio
and 1-2 injecti0118
o
may require surgical repair, i.e. acromiopiasty,
rotator cuff repair

Acromioclavicular (AC) Joint Pathology
·
2 main ligaments attach clavicle to scapula;
acromioclavicular (AC) and coracoclavicu1a (CC) lig8lllents
Mechanism
·
fall onto shoulder with adducted arm (fall onto tip
of shoulder)
Clinical Features
·
palpate step deformity between distal clavicle and
acromion (with dislocation)
·
pain with adduction of shoulder and/or palpation
over AC joint
·
limited ROM
Investigations
·
x-rays: AP, Zanca view (10-lSo cephalic tilt), axillary±
stress views (10 lb weight in patient's hand)
Treatment
·
non-operative (most-common): sling 1-3 weeks, ice,
analgesia
·
operative
o
indicati0118: AC and CC ligaments are both tom
and/or clavicle displaced posteriorly
o
procedure: excision ofclateral clavicle with ACJCC
ligament reconstruction
Clavicular Fracture
·
incidence proximal (5%), middle (80%), or distal
(IS%) third of clavicle
·
common in children (unites :rapidly without
complications)
Mechanism
·
fall on shoulder (8796), direct trauma to clavicle
(7%}, FOOSH (696)
Clinical Features
·
pain and tenting of skin
·
arm is clasped to chest to splint shoulder and
prevent movement
Treatment
·
evaluate neurovascular status of entire upper limb
·
proximal and middle third clavicular fractures
o
sling X 1-2 weeks
o
early ROM and strengthening once pain subsides
o
if ends overlap >2 cm. consider ORIF
·
distal third clavicular fractures
o
undisplaced (with ligaments intact): sling x 1-2
weeks
o
displaced (CC ligament injury): ORIF
Speciflc Complications (see
General Fracture Complications)
·
cosmetic bump usually only complication
·
shoulder stiffness, weakne511 with repetitive
activity
·
pneumothorax. injuries to brachial plexus and
subclavian vessel (all very rare)
Frozen Shoulder (Adhesive Capsulitis)
Definition
·
disorder characterized by progressive pain and
lrti1fneas of the shoulder usually resolving spontaneously after 18 months
Mechanism
·
primary adhesive capsulitis
o
idiopathic, usually ast1ociated with diabetes
mellitus
o
may resolve spontaneously in 9-18 months
·
secondary adhesive capsulitis
o
due to prolonged immobilization
o
shoulder-hand syndrome -type of chronic regional
pain syndrome (reflex sympathetic dystrophy) characterized by arm and shoulder
pain, decreased motion and diffuse swelling
o
following myocardia infarction, stroke, shoulder
trauma
Clinical Features
·
gradual onset (weeks to months) of diffuse
shoulder pain with:
• decreased active and passive ROM
• pain worse at night and often prevents
sleeping on affected side
• increased stiffness as pain subsides: continues
for 6-12 months after pain has disappeared
Investigations
·
x-nys may be normal, or may show demineralization
from disease
Treatment
·
active and passive ROM (physiotherapy)
·
NSAIDs and steroid injections if limited by pain
·
MUA (manipulation under aneathesia) and early
physiotherapy
·
arthroscopy for debridement/decompression
Related Topics