Chapter: Orthopaedics
Orthopaedics: Foot
Foot
Talar Fracture
Mechanism
·
axial loading or hyperdorsiflexion (MVA, fall from
a height)
·
60% of talus covered by articular cartilage
·
tenuous blood supply runs distal to proDma1 along
talar neck.
o
high risk of AVN with displaced fractures
Investigations
·
x-rays: AP, lateral
·
CT to better characterize fracture
·
MRI can clearly define extent of AVN
Treatment
·
undisplaced: non-weight bearing below knee cast x
20-24 weeks
·
displaced: ORIF (high rate of nonunion, AVN)
Calcaneal Fracture
Mechanism
·
axial loading: fall from a height onto heels
·
10% of fractures associated with compression
fractures of thoracic or lumbar spine
·
5% are bilateral
Physical Examination
·
swelling, bruising on heel/sole
·
wider, shortened, flatter heel when viewed from
behind
Investigations
·
x-rays: AP, lateral, oblique (Broden's view)
·
loss of Bohler's angle
·
CT - assess intraarticular extension
Treatment
·
closed vs. open reduction is controversial
·
non-weight bearing cast approximately 3 months
with early ROM and strengthening
Achilles Tendonitis
Mechanism
·
chronic inflammation from activity or poor-fitting
footwear
·
may also develop heel bumps
(retrocalcaneobursitis)
Physical Examination
·
pain, stiffness and crepitus with ROM
·
thickened tendon, palpable bump
Treatment
·
rest, NSAIDs
·
gentle stretching, deep tissue calf massage
·
orthotics, open back shoes
·
Do NOT inject steroids (risk of tendon rupture)
Achilles Tendon Rupture
Mechanism
·
loading activity, stop-and-go sports (e.g. squash,
tennis, basketball)
·
secondary to chronic tendonitis, steroid injection
Clinical Features
·
audible pop, sudden pain with push off movement
·
sensation of being kicked in heel when trying to plantar
flex
·
palpable gap
·
apprehensive toe off when walking
·
weak plantar flexion, +ve Thompson test: with
patient prone, squeezing the calf muscles should passively plantar flex the
foot to demonstrate intact Achilles tendon
o
+ve test = no passive plantar flexion = ruptured
tendon
Treatment
·
low demand or elderly: cast foot in plantar
flexion (to relax tendon) x 8-12 weeks
·
high demand: surgical repair, then cast as above x
6-8 weeks
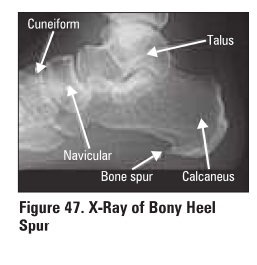
Plantar Fasciitis (Heal Spur Syndrome)
Mechanism
·
repetitive strain injury causing microtears and
inflammation of plantar fascia
·
female:male = 2:1
·
common in athletes (especially runners)
·
also associated with obesity, DM, seronegative and
seropositive arthritis
Clinical Features
·
morning pain and stiffness
·
intense pain when walking from rest that subsides
aa patient continues to walk
·
swelling, tenderness over sole
·
greatest at medial calcaneal tubercle and 1-2 cm
distal along plantar fascia
·
pain with toe dorsiflexion (stretches fascia)
Investigations
·
plain radiographs m rule out fractures
·
often see exostoses (heel spurs) at insertion
offilsda into medial calcaneal tubercle (see Figure 47)
·
spur is reactive to inflammation, not the cause of
pain
Treatment
·
rest, ice, NSAIDs, steroid injection
·
PT: stretching, ultrasound
·
orthotics with heel cup
o
to counteract pronation and disperse heel strike
forces
·
endoscopic surgical release of:lUcia in refractory
cases
o
spur removal is not required
Bunions (Hallux Valgus)
Mechanism
·
valgus alignment on 1st MTP (hallux valgus) causes
eccentric pull of extensor and intrinsic muscles
·
reactive exostosis forms with thickening of the skin
creating a bunion
·
most often associated with poor-fitting footwear
but can be hereditary
·
l0x more frequent in women
Clinical Features
·
painful bursa over medial eminence of 1st
metatarsal head
·
pronation (rotation inward) of great toe
·
numbness over medial aspect of great toe
Treatment
·
cosmetic and to relieve pain
·
non-operative first
o
properly fitted shoes low heel) and toe spacer
·
surgical
·
osteotomy with realignment of 1st MTP joint

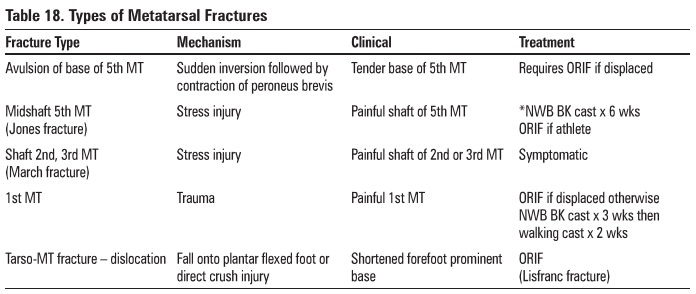
Metatarsal Fracture
·
as with the hand, 1st, 4th, 5th metatarsals (MT)
are relatively moblle, while the 2nd and 3rd are fixed (Table 18)
·
use Ottawa Foot Rules to determine need fur x-ray
Related Topics