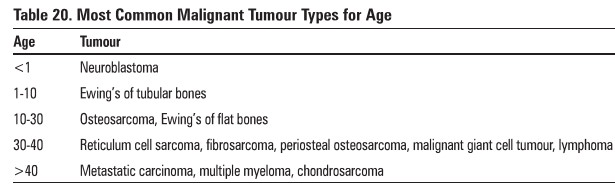
Chapter: Orthopaedics
Bone Tumours
Bone Tumours
·
primary bone tumours are rare after 3rd decade
·
metastases to bone are relatively common after 3rd
decade
Diagnosis
·
pain, swelling, rarely regional adenopathy
·
routine x-ray
o
location (which bone, diaphysis, metaphysis,
epiphysis)
o
size
o
lytic/lucent vs. scluotic
o
involvement (cortex, medulla, soft tissue)
o
matrix (radiolucent, radiodense or calcified)
o
periosteal reaction
o
margin (geographic n. permeative)
o
any pathological fracture
o
soft tissue swelling
·
malignancy is suggested by rapid growth, warmth,
tenderness, lack of sharp definition
·
staging should include
o
bloodwork Including liver enzymes
o
CT chest
o
bone scan
o
bone biopsy
o
––should be referred to specialized centre prior to
biopsy
o
––classified into benign, benign aggressive. and
malignant
·
MRl of affected bone
Benign Active Bone Tumours
1. Ostaold Osteoma
·
peak incidence in 2nd and 3rd decades, M:F = 3:1
·
small, round radiolucent nidus ( <1 cm)
surrounded by dense bone
o
tibia and femur most common
·
produces severe intermittent pain. mostly at night
(diurnal prostaglandin production)
·
characteristically relieved by NSAIDs
·
not known to metastasize
2. Osteochondroma
·
2nd and 3rd decades, M:F = 1.8:1
·
45% ofall benign bone tumours
·
metaphysis of long bone (distal ends of femur /proximal
ends of humerus)
o
cartilage-capped bony spur on surface of bone
('"mushroom" on x-ray)
o
may be multiple (hereditary, autosomal dominant
form) - higher risk of malignant change
·
generally very slow growing and asymptomatic
unless impinging on neurovascular structure
·
malignant degeneration occurs in 1-2% (becomes
painful or rapidly grows)
3. Enchondroma (Figure 54)
·
2nd and 3rd decades
·
50% occur in the small tubular bones of the hand
and foot; others in femur, humerus, ribs
·
benign cartilagenous growth, develops in medullary
cavity
o
single/multiple enlarged rarefied areas in tubular
bones
o
lytic lesion with sharp margination and central
calcification
·
malignant degeneration occurs in 1-296 (pain in
absence of pathologic fracture is an important clue)
·
not known to metastasize

4. Cystic Lesions
·
includes unicameral/solitary bone cyst (most
common), fibrous cortical defect
·
children and young adults
·
local pain. pathological fracture (50%
presentations) or incldental detection
o
lytic translucent area on metaphyseal side of
growth plate
o
cortex thinned/expanded; well defined lesion
·
aspiration cystic fluid: green/yellow colour with
high ALP
·
treatment of unicameral bone cyst with steroid
injections ± bone graft
Treatment
·
treatment only necessary if symptomatic
·
osteochondroma: resection
·
cystic lesions: currettage and bone graft
Benign Aggressive Bona Tumours
Giant Cell Tumours/Aneurysmal Bone Cyst/Osteoblastoma (Figure 55)
·
affects patients of skeletal maturity, peak 3rd decade
·
found in the distal femur, proximal tibia, distal
radius, sacrum, tarsal bones, spinal (osteoblastoma)
·
cortex appears thinned, expanded; well-demarcated
sclerotic margin; T2 MRI enhances fluid within lesion (hyper-intense signal)
·
local tenderness and swelling
·
15% recur within 2 years of surgery
·
giant cell tumour occasionally metastasizes (1-2%)

Treatment
·
intralesional curettage + bone graft or cement
·
wide local excision of expendable bones
Malignant Bone Tumours
1. Osteosarcoma (Figure
56)
·
most frequently diagnosed in 2nd decade of life
(60%)
·
history of Paget's disease radiation
·
predilection fur distal femur (45%), proximal
tibia (20%) and proximal hwnerus (15%)
o
invasive, variable histology; frequent metastases
without treatment Oung most common)
·
painful. poorly defined swelling. decreased ROM
·
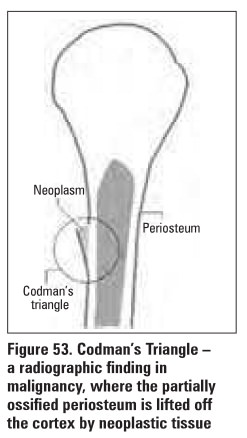
Hay shows Codman’s triangle (Figure 53)
o
––characteristic periosteal elevation and spicule
formation representing tumour extension into periosteum
o
destructive lesion in metaphysis may cross epiphyseal
plate
·
treatment: complete resection (limb salvage,
rarely amputation), neo-adjuvant cbemo
·
survival- 70%

2. Chondrosarcoma (Figure 57)
·
primary (2/3 cases)
o
previous normal bone, patient over 40; expands into
cortex to give pain, pathological fracture, flecks of calcification
·
secondary (1/3 cases)
o
––malignant degeneration of pre-existing cartilage
tumour such as enchondroma or osteochondroma, younger age group and better
prognosis than primary chondrosarcoma
·
most commonly occurs in pelvis, femur, ribs,
scapula, humerus (with metastasis to the hung)
·
unresponsive to chemotherapy, treat with
aggressive surgical resection+ reconstruction

3. Ewing's Sarcoma
·
most occur between 5-20 years old
·
florid periosteal reaction in diaphysis of long
bone
o
moth-eaten appearance with periosteal lamellated
pattern (onion-skinning)
·
present with mild fever, anemia, leukocytosis and
increased ESR/LDH
·
metastases frequent without treatment
·
treatment - resection, chemotherapy, radiation
·
survival- 70%
4. Multiple Myeloma
·
most common primary malignant tumour in adults
·
90% occur in people >40 years old
·
present with anemia, anorexia, renal failure,
nephritis, increased ESR, bone pain (cardinal early symptom), compression
fractures, hypercalcemia
·
high incidence of infections (e.g. pyelonephritis/pneumonia)
·
diagnosis
o
CT-guided biopsy of lytic lesions at multiple bony
sites
o
serum/urine protein electrophoresis
·
treatment chemotherapy, radiation, surgery for
symptomatic lesions or impending fractures
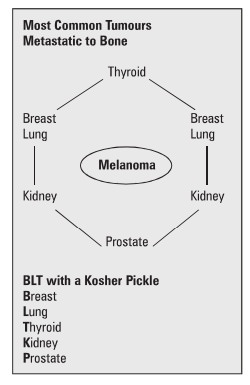
5. Bone Metastases
·
2/3 from breast or prostate; also consider
thyroid, lung, kidney
·
usually osteolytic; prostate occasionally
osteoblastic
·
bone scan for MSK involvement, MRI for spinal
involvement may be helpful
·
stabilization of impending fractures
o
internal fixation, IM rods
o
bone cement
Related Topics