Chapter: Basic & Clinical Pharmacology : Cancer Chemotherapy
Fluoropyrimidines
FLUOROPYRIMIDINES
5-Fluorouracil
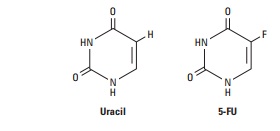
5-Fluorouracil (5-FU) is inactive in its parent form and requires activation via a complex series of enzymatic reactions to ribosyl and deoxyribosyl nucleotide metabolites. One of these metabo-lites, 5-fluoro-2′-deoxyuridine-5′-monophosphate (FdUMP), forms a covalently bound ternary complex with the enzyme thy-midylate synthase and the reduced folate 5,10-methylenetetrahy-drofolate, a reaction critical for the de novo synthesis of thymidylate. This results in inhibition of DNA synthesis through “thymineless death.” 5-FU is converted to 5-fluorouridine-5′-triphosphate (FUTP), which is then incorporated into RNA, where it interferes with RNA processing and mRNA translation. 5-FU is also converted to 5-fluorodeoxyuridine-5′-triphosphate (FdUTP), which can be incorporated into cellular DNA, resulting in inhibition of DNA synthesis and function. Thus, the cytotoxic-ity of 5-FU is thought to be the result of combined effects on both DNA- and RNA-mediated events.
5-FU is administered intravenously, and the clinical activity of this drug is highly schedule-dependent. Because of its extremely short half-life, on the order of 10–15 minutes, infusional schedules of administration have been generally favored over bolus schedules. Up to 80–85% of an administered dose of 5-FU is catabolized by the enzyme dihydropyrimidine dehydrogenase (DPD). Of note, a pharmacogenetic syndrome involving partial or complete defi-ciency of the DPD enzyme is seen in up to 5% of cancer patients; in this setting, severe toxicity in the form of myelosuppression, diarrhea, nausea and vomiting, and neurotoxicity is observed.
5-FU remains the most widely used agent in the treatment of colorectal cancer, both as adjuvant therapy and for advanced disease. It also has activity against a wide variety of solid tumors, including cancers of the breast, stomach, pancreas, esophagus, liver, head and neck, and anus. Major toxicities include myelosuppression, gastro-intestinal toxicity in the form of mucositis and diarrhea, skin toxic-ity manifested by the hand-foot syndrome, and neurotoxicity.
Capecitabine
Capecitabine is a fluoropyrimidine carbamate prodrug with 70–80% oral bioavailability. It undergoes extensive metabolism in the liver by the enzyme carboxylesterase to an intermediate, 5′-deoxy-5-fluorocytidine. This metabolite is then converted to 5′-deoxy-5-fluorouridine by the enzyme cytidine deaminase. These two initial steps occur mainly in the liver. The 5′-deoxy-5-fluorouridine metabolite is finally hydrolyzed by thymidine phos-phorylase to 5-FU directly in the tumor. The expression of thymidine phosphorylase has been shown to be significantly higher in a broad range of solid tumors than in corresponding normal tissue, particularly in breast cancer and colorectal cancer.
This oral fluoropyrimidine is used in the treatment of meta-static breast cancer either as a single agent or in combination with other anticancer agents, including docetaxel, paclitaxel, lapatinib, ixabepilone, and trastuzumab. It is also approved for use in the adjuvant therapy of stage III and high-risk stage II colon cancer as well as for treatment of metastatic colorectal cancer as monother-apy. At this time, significant efforts are directed at combining this agent with other active cytotoxic agents, including irinotecan and oxaliplatin. In Europe and Asia, the capecitabine/oxaliplatin (XELOX) regimen is approved for the first-line treatment of meta-static colorectal cancer, and this regimen is now widely used in the USA. The main toxicities of capecitabine include diarrhea and the hand-foot syndrome. While myelosuppression, nausea and vomit-ing, and mucositis are also observed with this agent, their incidence is significantly less than that observed with intravenous 5-FU.
Related Topics