Chapter: Medical Surgical Nursing: Vascular Disorders and Problems of Peripheral Circulation
Anatomy of the Vascular System
ANATOMY
OF THE VASCULAR SYSTEM
Arteries and Arterioles
Arteries are thick-walled structures that carry blood from the heart to the tissues. The aorta, which has a diameter of approxi-mately 25 mm (1 inch), gives rise to numerous branches, which divide into smaller arteries that are about 4 mm (0.16 inch) in diameter by the time they reach the tissues. Within the tissues, the vessels divide further, diminishing to approximately 30 ÎĽ m in diameter; these vessels are called arterioles.
The
walls of the arteries and arterioles are composed of three layers: the intima,
an inner endothelial cell layer; the media, a middle layer of smooth elastic
tissue; and the adventitia, an outer layer of connective tissue. The intima, a
very thin layer, provides a smooth surface for contact with the flowing blood.
The media makes up most of the vessel wall in the aorta and other large
ar-teries of the body. This layer is composed chiefly of elastic and connective
tissue fibers that give the vessels considerable strength and allow them to
constrict and dilate to accommodate the blood ejected from the heart (stroke
volume) and maintain an even, steady flow of blood. The adventitia is a layer
of connective tis-sue that anchors the vessel to its surroundings. There is
much less elastic tissue in the smaller arteries and arterioles, and the media
in these vessels is composed primarily of smooth muscle.
Smooth
muscle controls the diameter of the vessels by con-tracting and relaxing.
Chemical, hormonal, and nervous system factors influence the activity of smooth
muscle. Because arterioles can alter their diameter, thereby offering
resistance to blood flow, they are often referred to as resistance vessels. Arterioles regulate the volume and pressure in
the arterial system and the rate of blood flow to the capillaries. Because of
the large amount of mus-cle, the walls of the arteries are relatively thick,
accounting for ap-proximately 25% of the total diameter of the artery. The
walls of the arterioles account for approximately 67% of the total diame-ter of
arterioles.
The
intima and the inner third of the smooth muscle layer are in such close contact
with the blood that the blood vessel receives its nourishment by direct
diffusion. The adventitia and the outer media layers have a limited vascular
system for nourishment and require their own blood supply to meet metabolic
needs.
Capillaries
Capillary
walls, which lack smooth muscle and adventitia, are composed of a single layer
of endothelial cells. This thin-walled structure permits rapid and efficient
transport of nutrients to the cells and removal of metabolic wastes. The
diameter of capillar-ies ranges from 5 to 10 ÎĽ m;
this narrow channel requires red blood cells to alter their shape to pass
through these vessels. Changes in a capillary’s diameter are passive and are
influenced by contractile changes in the blood vessels that carry blood to and
from a capillary. The capillary’s diameter also changes in response to chemical
stimuli. In some tissues, a cuff of smooth muscle, called the precapillary
sphincter, is located at the arteriolar end of the capillary and is
responsible, along with the arteriole, for con-trolling capillary blood flow.
Some
capillary beds, such as in the fingertips, contain arte-riovenous anastomoses,
through which blood passes directly from the arterial to the venous system.
These vessels are believed to regulate heat exchange between the body and the
external environment.
The
distribution of capillaries varies with the type of tissue. For example,
skeletal tissue, which is metabolically active, has a denser capillary network
than does cartilage, which is less active.
Veins and Venules
Capillaries
join to form larger vessels called venules, which join to form veins. The
venous system is therefore structurally analo-gous to the arterial system;
venules correspond to arterioles, veins to arteries, and the vena cava to the
aorta. Analogous types of vessels in the arterial and venous systems have
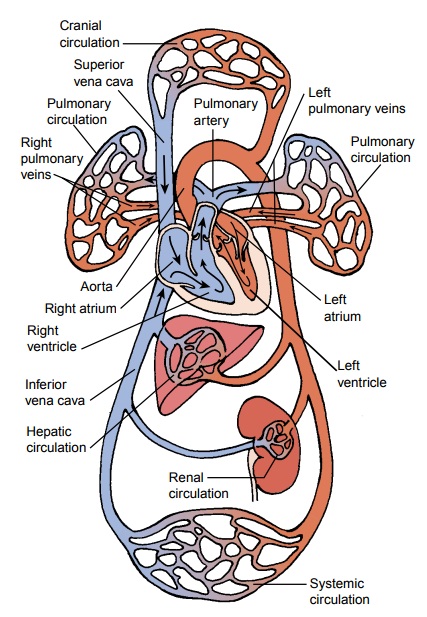
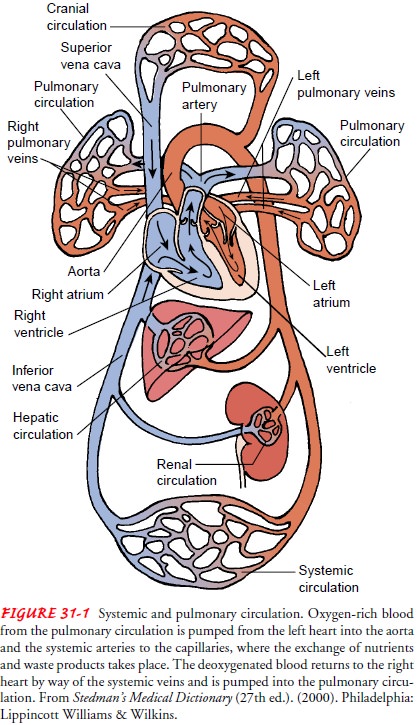
approximately the same diameters (see Fig. 31-1).
The
walls of the veins, in contrast to those of the arteries, are thinner and
considerably less muscular. The wall of the average vein amounts to only 10% of
the vein diameter, in contrast to 25% in the artery. The walls of a vein, like
those of arteries, are com-posed of three layers, although these layers are not
as well defined.
The
thin, less muscular structure of the vein wall allows these vessels to distend
more than arteries. Greater distensibility and compliance permit large volumes
of blood to be stored in the veins under low pressure. For this reason, veins
are referred to as capacitance vessels.
Approximately 75% of total blood volume iscontained in the veins. The
sympathetic nervous system, which innervates the vein musculature, can
stimulate the veins to con-strict (venoconstriction), thereby reducing venous
volume and increasing the volume of blood in the general circulation.
Con-traction of skeletal muscles in the extremities creates the primary pumping
action to facilitate venous blood flow back to the heart.
Some
veins, unlike arteries, are equipped with valves. In gen-eral, veins that
transport blood against the force of gravity, as in the lower extremities, have
one-way bicuspid valves that interrupt the column of blood to prevent blood
from seeping backward as it is propelled toward the heart. Valves are composed
of endo-thelial leaflets, the competency of which depends on the integrity of the
vein wall.
Lymphatic Vessels
The
lymphatic vessels are a complex network of thin-walled vessels similar to the
blood capillaries. This network collects lymphatic fluid from tissues and
organs and transports the fluid to the venous circulation. The lymphatic
vessels converge into two main struc-tures: the thoracic duct and the right
lymphatic duct. These ducts empty into the junction of the subclavian and the
internal jugular veins. The right lymphatic duct conveys lymph primarily from
the right side of the head, neck, thorax, and upper arms. The thoracic duct
conveys lymph from the remainder of the body. Peripheral lymphatic vessels join
larger lymph vessels and pass through re-gional lymph nodes before entering the
venous circulation. The lymph nodes play an important role in filtering foreign
particles.
The
lymphatic vessels are permeable to large molecules and provide the only means
by which interstitial proteins can return to the venous system. With muscular
contraction, lymph vessels become distorted to create spaces between the
endothelial cells, allowing protein and particles to enter. Muscular
contraction of the lymphatic walls and surrounding tissues aids in propelling
the lymph toward the venous drainage points.
Related Topics