Chapter: Medical Surgical Nursing: Vascular Disorders and Problems of Peripheral Circulation
Leg Ulcers
LEG
ULCERS
A leg
ulcer is an excavation of the skin surface that occurs when inflamed necrotic
tissue sloughs off. About 75% of all leg ulcers result from chronic venous
insufficiency. Lesions due to arterial insufficiency account for approximately
20%; the remaining 5% are caused by burns, sickle cell anemia, and other
factors (Gloviczki & Yao, 2001).
Pathophysiology
Inadequate
exchange of oxygen and other nutrients in the tissue is the metabolic
abnormality that underlies the development of leg ulcers. When cellular
metabolism cannot maintain energy bal-ance, cell death (necrosis) results.
Alterations in blood vessels at the arterial, capillary, and venous levels may
affect cellular processes and lead to the formation of ulcers.
Clinical Manifestations
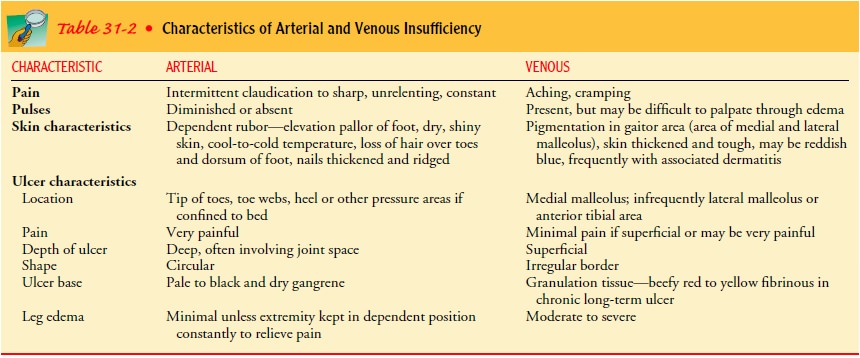
The
clinical appearance and associated characteristics of leg ulcers are determined
by the cause of the ulcer. Most ulcers, especially in an elderly patient, have
more than one cause. The symptoms depend on whether the problem is arterial or
venous in origin (see Table 31-2). The severity of the symptoms depends on the
extent and duration of the vascular insufficiency. The ulcer itself appears as
an open, inflamed sore. The area may be draining or covered by eschar (dark,
hard crust).
ARTERIAL ULCERS
Chronic arterial disease is characterized by intermittent claudica-tion, which is pain caused by activity and relieved after a few min-utes of rest. The patient may also complain of digital or forefoot pain at rest. If the onset of arterial occlusion is acute, ischemic pain is unrelenting and rarely relieved even with opioid analgesics. Typically, arterial ulcers are small, circular, deep ulcerations on the tips of toes or in the web spaces between toes. Ulcers often occur on the medial side of the hallux or lateral fifth toe and may be caused by a combination of ischemia and pressure (Fig. 31-17).

Arterial
insufficiency may result in gangrene of the toe (digi-tal gangrene), which
usually is caused by trauma. The toe is stubbed and then turns black (see Fig.
31-17). Usually, patients with this problem are elderly people without adequate
circulation to provide revascularization. DĂ©bridement is contraindicated in
these instances. Although the toe is gangrenous, it is dry. Man-aging dry
gangrene is preferable to débriding the toe and causing an open wound that will
not heal because of insufficient circula-tion. If the toe were to be amputated,
the lack of adequate circu-lation would prevent healing and might make further
amputation necessary—a below-knee or an above-knee amputation. A higher-level
amputation in the elderly could result in a loss of indepen-dence and possibly
institutional care. Dry gangrene of the toe in an elderly person with poor
circulation is usually left undisturbed. The nurse keeps the toe clean and dry
until it separates (without creating an open wound).
VENOUS ULCERS
Chronic
venous insufficiency is characterized by pain described as aching or heaviness.
The foot and ankle may be edematous. Ulcerations are in the area of the medial
or lateral malleolus (gaiter area) and are typically large, superficial, and
highly exuda-tive. Venous hypertension causes extravasation of blood, which
discolors the gaiter area (see Fig. 31-17). Patients with neuropa-thy
frequently have ulcerations on the side of the foot over the metatarsal heads.
Assessment and Diagnostic Findings
Because
ulcers have many causes, the cause of each ulcer needs to be identified so
appropriate therapy can be prescribed. The his-tory of the condition is
important in determining venous or arte-rial insufficiency. The pulses of the
lower extremities (femoral, popliteal, posterior tibial, and dorsalis pedis)
are carefully exam-ined. More conclusive diagnostic aids are Doppler and duplex
ultrasound studies, arteriography, and venography. Cultures of the ulcer bed
may be necessary to determine whether the infect-ing agent is the primary cause
of the ulcer.
Medical Management
Patients
with ulcers can be effectively managed by advanced prac-tice nurses or
certified wound care nurses in collaboration with physicians. All ulcers have
the potential to become infected.
PHARMACOLOGIC THERAPY
Antibiotic
therapy is prescribed when the ulcer is infected; the specific antibiotic is
selected on the basis of culture and sensitiv-ity test results. Oral
antibiotics usually are prescribed because top-ical antibiotics have not proven
to be effective for leg ulcers.
DÉBRIDEMENT
To
promote healing, the wound is kept clean of drainage and necrotic tissue. The
usual method is to flush the area with nor-mal saline solution. If this is
unsuccessful, débridement may be necessary. Débridement is the removal of
nonviable tissue from wounds. Removing the dead tissue is important,
particularly in instances of infection. DĂ©bridement can be accomplished by
several different methods:
•
Sharp surgical débridement is the fastest method and can be performed by a
physician, skilled advanced practice nurse, or certified wound care nurse in
collaboration with the physician.
•
Nonselective débridement can be accomplished by applying isotonic saline
dressings of fine-mesh gauze to the ulcer. When the dressing dries, it is
removed (dry), along with the debris adhering to the gauze. Pain management is
usually necessary.
•
Enzymatic débridement with the application of enzyme ointments may be
prescribed to treat the ulcer. The ointment is applied to the lesion but not to
normal surrounding skin. Most enzymatic ointments are covered with
saline-soaked gauze that has been thoroughly wrung out. A dry gauze dressing
and a loose bandage are then applied. The enzymatic ointment is discontinued
when the necrotic tissue has been débrided and an appropriate wound dressing is
applied.
•
DĂ©briding agents can be used. Dextranomer (Debrisan) beads are small, highly
porous, spherical beads (0.1 to 0.3 mm in diameter) that can absorb wound
secretions. Bacteria and the products of tissue necrosis and protein
degradation are absorbed into the bead layer. When the beads are saturated,
they take on a grayish yellow color, at which point their cleansing action
stops. They are then flushed from the wound with normal saline, and a fresh
layer is applied.
•
Calcium alginate dressings can also be used for débridement when absorption of
exudate is needed. These dressings are changed when the exudate seeps through
the cover dressing or at least every 7 days. The dressing can also be used on
areas that are bleeding, because the material helps stop the bleeding. As the
dry fibers absorb exudate, they become a gel that is painlessly removed from
the ulcer bed. Calcium alginate dressings should not be used on dry or
nonexudative wounds.
TOPICAL THERAPY
A
variety of topical agents can be used in conjunction with cleans-ing and
débridement therapies to promote healing of leg ulcers. The goals of treatment
are to remove devitalized tissue and to keep the ulcer clean and moist while
healing takes place. The treatment should not destroy developing tissue. For
topical treatments to be successful, adequate nutritional therapy must be
maintained.
WOUND DRESSING
After
the circulatory status has been assessed and determined to be adequate for
healing (ABI of more than 0.5), surgical dressings can be used to promote a
moist environment. The simplest method is to use a wound contact material (eg,
Tegapore) next to the wound bed and cover it with gauze. Tegapore maintains a
moist environment, can be left in place for several days, and does not disrupt
the capillary bed when removed for evaluation. Hydrocolloids (eg, Comfeel,
DuoDerm CGF, Restore, Tegasorb) are also available options to promote
granulation tissue and re-epithelialization. They also provide a barrier for
protection because they adhere to the wound bed and surrounding tissue.
However, deep wounds and infected wounds are often more appropriately treated
with other dressings.
Knowledge
deficit, frustration, fear, and depression can result in the patient’s and
family’s decreased compliance with the pre-scribed therapy; therefore, patient
and family education is neces-sary before beginning and throughout the wound
care program.
STIMULATED HEALING
Tissue-engineered
human skin equivalent along with therapeutic compression has been developed by
Apligraf; it is a skin product cultured from human dermal fibroblasts and
keratinocytes. When applied, it seems to react to factors in the wound and may
inter-act with the patient’s cells to stimulate the production of growth
factors. Application is not difficult, no suturing is involved, and the
procedure is painless.
Related Topics