Chapter: Medical Surgical Nursing: Vascular Disorders and Problems of Peripheral Circulation
Peripheral Arterial Occlusive Disease
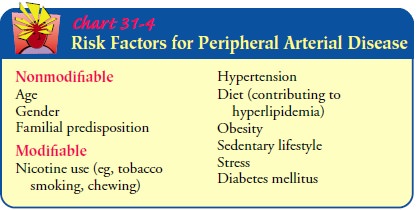
PERIPHERAL
ARTERIALOCCLUSIVE DISEASE
Arterial
insufficiency of the extremities is usually found in indi-viduals older than 50
years of age, most often in men. The legs are most frequently affected;
however, the upper extremities may be involved. The age of onset and the
severity are influenced by the type and number of atherosclerotic risk factors
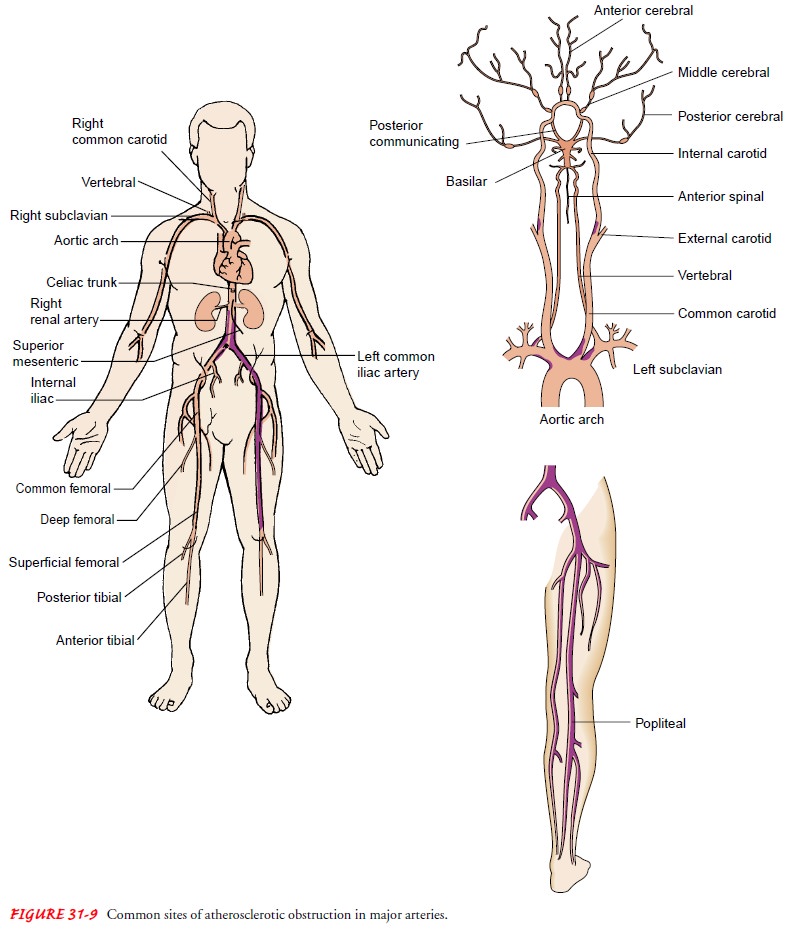
(Chart 31-4). In peripheral arterial disease, obstructive lesions are
predomi-nantly confined to segments of the arterial system extending from the
aorta below the renal arteries to the popliteal artery (Fig. 31-9). However,
distal occlusive disease is frequently seen in patients with diabetes mellitus
and in elderly patients.
Clinical Manifestations
The
hallmark is intermittent claudication. This pain may be de-scribed as aching,
cramping, fatigue, or weakness that is consis-tently reproduced with the same
degree of exercise or activity and relieved with rest. The pain commonly occurs
in muscle groups one joint level below the stenosis or occlusion. As the
disease progresses, the patient may have a decreased ability to walk the same
distance or may notice increased pain with am-bulation. When the arterial
insufficiency becomes severe, the patient begins to have rest pain. This pain
is associated with critical ischemia of the distal extremity and is persistent,
aching, or boring; it may be so excruciating that it is unrelieved by opi-oids.
Ischemic rest pain is usually worse at night and often wakes the patient.
Elevating the extremity or placing it in a hor-izontal position increases the
pain, whereas placing the extrem-ity in a dependent position reduces the pain.
In bed, some patients sleep with the affected leg hanging over the side of the
bed. Some patients sleep in a reclining chair in an attempt to re-lieve the
pain.
Assessment and Diagnostic Findings
A
sensation of coldness or numbness in the extremities may ac-company
intermittent claudication and is a result of the reduced arterial flow. When
the extremity is examined, it may feel cool to the touch and look pale when
elevated or ruddy and cyanotic when placed in a dependent position. Skin and
nail changes, ulcerations, gangrene, and muscle atrophy may be evident. Bruits
may be auscultated with a stethoscope; a bruit is the sound produced by
turbulent blood flow through an irregular, tortuous, stenotic vessel or through
a dilated segment of the vessel (aneurysm). Peripheral pulses may be diminished
or absent.
Examining
the peripheral pulses is an important part of assess-ing arterial occlusive
disease. Unequal pulses between extremities or the absence of a normally
palpable pulse is a sign of peripheral arterial disease. The femoral pulse in
the groin and the posterior tibial pulse beside the medial malleolus are most
easily palpated. The popliteal pulse is sometimes difficult to palpate; the
location of the dorsalis pedis artery on the dorsum of the foot varies and is
normally absent in about 7% of the population.
The
presence, location, and extent of arterial occlusive disease are determined by
a careful history of the symptoms and by phys-ical examination. The color and
temperature of the extremity are noted and the pulses palpated. The nails may
be thickened and opaque, and the skin may be shiny, atrophic, and dry, with
sparse hair growth. The assessment includes comparison of the right and left
extremities.
The
diagnosis of peripheral arterial occlusive disease may be made using CW Doppler
and ankle-brachial indices (ABIs), tread-mill testing for claudication, duplex
ultrasonography, or other imaging studies previously described.
Medical Management
Generally,
patients feel better with some type of exercise pro-gram. If this program is
combined with weight reduction and ces-sation of tobacco use, patients often
can improve their activity tolerance. Patients should not be promised that
their symptoms will be relieved if they stop tobacco use, because claudication
may persist, and they may lose their motivation to stop using tobacco.
PHARMACOLOGIC THERAPY
Various
medications are prescribed to treat the symptoms of pe-ripheral arterial
disease. Pentoxifylline (Trental) increases ery-throcyte flexibility and
reduces blood viscosity, and it is therefore thought to improve the supply of
oxygenated blood to the mus-cle. Cilostazol (Pletal) works by inhibiting
platelet aggregation, inhibiting smooth muscle cell proliferation, and
increasing vaso-dilation. Antiplatelet aggregating agents such as aspirin,
ticlopi-dine (Ticlid), and clopidogrel (Plavix) are thought to improve
circulation throughout diseased arteries or prevent intimal hyper-plasia
leading to stenosis.
SURGICAL MANAGEMENT
In most patients, when intermittent claudication becomes severe and disabling or when the limb is at risk for amputation because of tissue loss, vascular grafting or endarterectomy is the treatment of choice. The choice of the surgical procedure depends on the degree and location of the stenosis or occlusion. Other important considerations are the overall health of the patient and the length of the procedure that can be tolerated. It is sometimes necessary to provide the palliative therapy of primary amputation rather than an arterial bypass. If endarterectomy is performed, an inci-sion is made into the artery, and the atheromatous obstruction is removed. The artery is then sutured closed to restore vascular in-tegrity (Fig. 31-10).
Bypass
grafts are performed to reroute the blood flow around the stenosis or
occlusion. Before bypass grafting, the surgeon de-termines where the distal anastomosis (site where the vessels are
surgically joined) will be placed. The distal outflow vessel must be at least
50% patent for the graft to remain patent. A higher by-pass graft patency rate
is associated with keeping the length of the bypass as short as possible.
If the
atherosclerotic occlusion is below the inguinal ligament in the superficial
femoral artery, the surgical procedure of choice is the femoral-to-popliteal
graft. This procedure is further classified as above-knee and below-knee
grafts, referring to the location of the distal anastomosis.
Lower leg or ankle vessels with occlusions may also require grafts. Occasionally, the entire popliteal artery is occluded, and there is only collateral circulation. The distal anastomosis may be made onto any of the tibial arteries (posterior tibial, anterior tib-ial, or peroneal arteries) or the dorsalis pedis or plantar artery.
The distal
anastomosis site is determined by the ease of exposure of the vessel in surgery
and by which vessel provides the best flow to the distal limb. These grafts
require the use of native vein to en-sure patency. Native vein is autologous
vein (the patient’s own vein). The greater or lesser saphenous vein or a
combination of one of the saphenous veins and an upper extremity vein such as
the cephalic vein are used to meet the required length.
How
long the graft remains patent is determined by several fac-tors, including the
size of the graft, graft location, and develop-ment of intimal hyperplasia at
anastomosis sites. Bypass grafts may be synthetic or autologous vein. Several
synthetic materials are available for use as a peripheral bypass graft: woven
or knitted Dacron, expanded polytetrafluoroethylene (ePTFE, such as Gore-Tex or
Impra), collagen-impregnated, and umbilical vein. Infec-tion is a problem that
threatens survival of the graft and almost always requires removal of the
graft.
If a
vein graft is the surgical choice, care must be taken in the operating room not
to damage the vein after harvesting (removing the vein from the patient’s
body). The vein is occluded at one end and inflated with a heparinized solution
to check for leakage and competency. When this is done, the graft is placed in
a heparinized solution to keep it from becoming dry and brittle.
Nursing Management
MAINTAINING CIRCULATION
The
primary objective in the postoperative management of patients who have
undergone vascular procedures is to maintain adequate circulation through the
arterial repair. Pulses, Doppler assessment, color and temperature of the extremity,
capillary refill, and sensory and motor function of the affected extremities
are checked, com-pared with those of the other extremity, and recorded every
hour for the first 8 hours and then every 2 hours for 24 hours. Doppler
eval-uation of the vessels distal to the bypass graft should be performed for
all postoperative vascular patients, because it is more sensitive than
palpation for pulses. The ABI is monitored at least once every 8 hours for the
first 24 hours and then once each day until discharge (not usually assessed for
pedal artery bypasses). An adequate circu-lating blood volume should be
established and maintained. Disap-pearance of a pulse that was present may
indicate thrombotic occlusion of the graft; the surgeon is immediately notified.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Continuous
monitoring of urine output (more than 30 mL/hour), central venous pressure,
mental status, and pulse rate and volume permit early recognition and treatment
of fluid imbalances. Bleed-ing can result from the heparin administered during
surgery or from an anastomotic leak. A hematoma may form as well.
Leg
crossing and prolonged extremity dependency are avoided to prevent thrombosis.
Edema is a normal postoperative finding; however, elevating the extremities and
encouraging the patient to exercise the extremities while in bed reduces edema.
Elastic com-pression stockings may be prescribed for some patients, but care
must be taken to avoid compressing distal vessel bypass grafts. Se-vere edema
of the extremity, pain, and decreased sensation of toes or fingers can be an
indication of compartment syndrome.
PROMOTING HOME AND COMMUNITY-BASED CARE
Discharge
planning includes assessing the patient’s ability to manage independently. The
nurse determines if the patient has a network of family and friends to assist
with activities of daily liv-ing. The patient may need to be encouraged to make
the lifestyle changes necessary with a chronic disease, including pain
man-agement and modifications in diet, activity, and hygiene (skin care). The
nurse ensures that the patient has the knowledge and ability to assess for any
postoperative complications such as in-fection, occlusion of the artery or
graft, and decreased blood flow. The nurse assists the patient in developing a
plan to stop using tobacco. The Plan of Nursing Care describes nursing care for
patients with peripheral vascular disease.
UPPER EXTREMITY ARTERIAL OCCLUSIVE DISEASE
Arterial
occlusions occur less frequently in the upper extremities (arms) than in the
legs and cause less severe symptoms because the collateral circulation is
significantly better in the arms. The arms also have less muscle mass and are
not subjected to the work-load of the legs.
Clinical Manifestations
Stenosis
and occlusions in the upper extremity result from ather-osclerosis or trauma.
The stenosis usually occurs at the origin of the vessel proximal to the
vertebral artery, setting up the vertebral artery as the major contributor of
flow. The patient may develop a “subclavian steal” syndrome characterized by
reverse flow in the vertebral and basilar artery to provide blood flow to the
arm. This syndrome may cause vertebrobasilar (cerebral) symptoms. Most patients
are asymptomatic; however, some report vertigo, ataxia, syncope, or bilateral
visual changes.
The
patient typically complains of arm fatigue and pain with exercise (forearm
claudication) and inability to hold or grasp ob-jects (eg, painting, combing
hair, placing objects on shelves above the head). Some even notice difficulties
driving.
Assessment and Diagnostic Findings
Assessment findings include coolness and
pallor of the affected ex-tremity, decreased capillary refill, and a difference
in arm blood pressures of more than 20 mm Hg. Noninvasive studies performed to
evaluate for upper extremity arterial occlusions include upper and forearm
blood pressure determinations and duplex ultrasonography to identify the
anatomic location of the lesion and to evaluate the hemodynamics of the blood
flow. Transcranial Doppler evaluation is performed to evaluate the intracranial
circulation and to detect any siphoning of blood flow from the posterior
circulation to pro-vide blood flow to the affected arm. If a surgical or
interventional procedure is planned, an arteriogram may be necessary.
Medical Management
If a
short, focal lesion is identified in an upper extremity artery, a PTA may be
performed. If the lesion involves the subclavian artery with documented
siphoning of blood flow from the intracranial cir-culation, several surgical
procedures are available: carotid–to–sub-clavian artery bypass,
axillary–to–axillary artery bypass, and autogenous reimplantation of the
subclavian to the carotid artery.
Nursing Management
Nursing
assessment involves bilateral comparison of upper arm blood pressures (obtained
by stethoscope and Doppler); radial, ulnar, and brachial pulses; motor and
sensory function; tempera-ture; color changes; and capillary refill every 2
hours. Disappear-ance of a pulse or Doppler flow that had been present may indicate
an acute occlusion of the vessel, and the physician is notified immediately.
After
surgery, the arm is kept at heart level or elevated, with the fingers at the
highest level. Pulses are monitored with Doppler assessment of the arterial
flow every hour for 8 hours and then every 2 hours for 24 hours. Blood pressure
(obtained by stetho-scope and Doppler) is also assessed every hour for 8 hours
and then every 2 hours for 24 hours. Motor and sensory function, warmth, color,
and capillary refill are monitored with each arte-rial flow (pulse) assessment.
Discharge
planning includes assessing the patient’s ability to manage independently. The
nurse determines whether the pa-tient has a network of family and friends to
assist with activities of daily living. The patient may need to be encouraged
to make the lifestyle changes necessary for a chronic disease, including pain
management and modifications in diet, activity, and hygiene(skin care). The
nurse ensures that the patient has the knowledge and ability to assess for any
postoperative complications such as infection, reocclusion of the artery or
occlusion of the graft, and decreased blood flow. The patient is assisted in
developing a plan to stop using tobacco. The Plan of Nursing Care describes
nursing care for patients with peripheral vascular disease.
Related Topics