Chapter: Medical Surgical Nursing: Vascular Disorders and Problems of Peripheral Circulation
Assessment of Vascular Disorders: Health History and Clinical Manifestations
Assessment
HEALTH
HISTORY AND CLINICAL MANIFESTATIONS
A
description of the pain and any precipitating factors, the skin color and
temperature, and the peripheral pulses are important for the diagnosis of
arterial disorders.
Intermittent Claudication
muscular,
cramp-type pain in the extremities consistently re-produced with the same
degree of exercise or activity and relieved by rest is experienced by patients
with peripheral arterial insuffi-ciency. Referred to as intermittent claudication, this pain is caused by the inability of
the arterial system to provide adequate blood flow to the tissues in the face
of increased demands for nu-trients during exercise. As the tissues are forced
to complete the energy cycle without the nutrients, muscle metabolites and
lactic acid are produced. Pain is experienced as the metabolites aggra-vate the
nerve endings of the surrounding tissue. Usually, about 50% of the arterial
lumen or 75% of the cross-sectional area must be obstructed before intermittent
claudication is experienced. When the patient rests and thereby decreases the
metabolic needs of the muscles, the pain subsides. The progression of the
arterial disease can be monitored by documenting the amount of exercise or the
distance a patient can walk before pain is produced. Per-sistent pain in the
forefoot when the patient is resting indicates a severe degree of arterial
insufficiency and a critical state of is-chemia. Known as rest pain, this discomfort is often worse at night and may
interfere with sleep. This pain frequently requires that the extremity be
lowered to a dependent position to improve perfusion pressure to the distal
tissues.
The
site of arterial disease can be deduced from the location of claudication,
because pain occurs in muscle groups below the disease. As a general rule, the
pain of intermittent claudication occurs one joint level below the disease
process. Calf pain may ac-company reduced blood flow through the superficial
femoral or popliteal artery, whereas pain in the hip or buttock may result from
reduced blood flow in the abdominal aorta or the common iliac or hypogastric
arteries.
Changes in Skin Appearance and Temperature
Adequate
blood flow warms the extremities and gives them a rosy coloring. Inadequate
blood flow results in cool and pale extrem-ities. Further reduction of blood
flow to these tissues, which oc-curs when the extremity is elevated, for
example, results in an even whiter or more blanched appearance (pallor). Rubor, a reddish blue discoloration of
the extremities, may be observed within 20 seconds to 2 minutes after the
extremity is dependent. Rubor suggests severe peripheral arterial damage in
which vessels that cannot constrict remain dilated. Even with rubor, the
ex-tremity begins to turn pale with elevation. Cyanosis, a bluish tint on the
skin, is manifested when the amount of oxygenated hemo-globin contained in the
blood is reduced.
Additional changes resulting from a chronically reduced nutri-ent supply include loss of hair, brittle nails, dry or scaling skin, atrophy, and ulcerations. Edema may be apparent bilaterally or unilaterally and is related to the affected extremityÔÇÖs chronically de-pendent position because of severe rest pain. Gangrenous changes appear after prolonged, severe ischemia and represent tissue necro-sis. In elderly patients who are inactive, gangrene may be the first sign of disease. These patients may have adjusted their lifestyle to accommodate the limitations imposed by the disease, and may not walk enough to develop symptoms of claudication. Cir-culation is decreased, but this is not apparent to the patient until trauma occurs. At this point, gangrene develops when minimal arterial flow is impaired further by edema formation resulting from the traumatic event.
Pulses
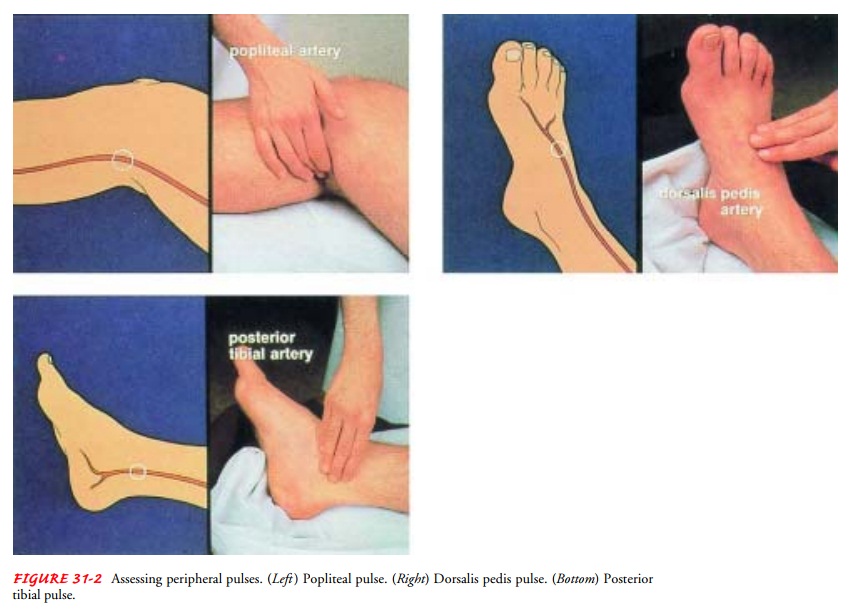
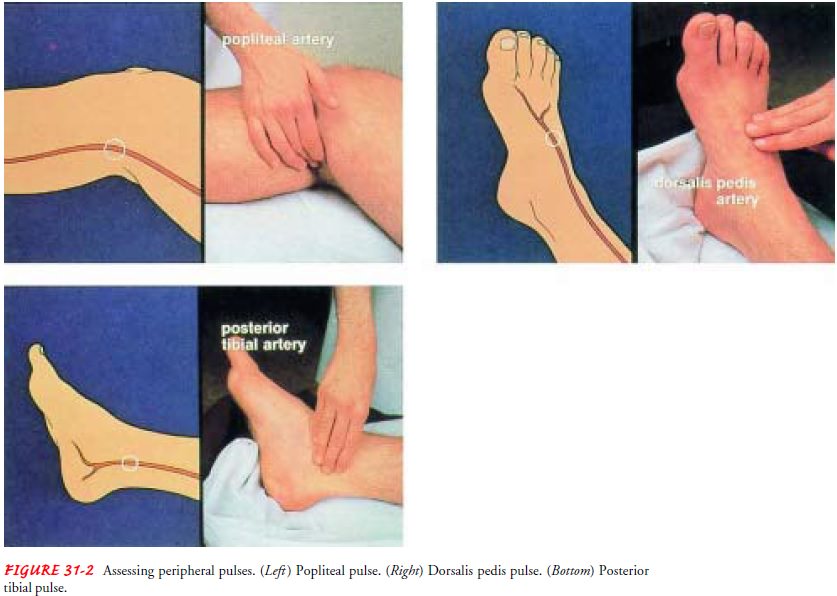
Determining
the presence or absence, as well as the quality, of peripheral pulses is
important in assessing the status of peripheral arterial circulation (Fig.
31-2). Absence of a pulse may indicate that the site of stenosis (narrowing or constriction) is proximal to that location.
Occlusive arterial disease impairs blood flow and can reduce or obliterate
palpable pulsations in the extremities. Pulses should be palpated bilaterally
and simultaneously, com-paring both sides for symmetry in rate, rhythm, and
quality.
Gerontologic Considerations
In
elderly people, symptoms of peripheral arterial disease may be more pronounced
than in younger people because of the con-ditionÔÇÖs duration and coexisting
chronic disease. Intermittent claudication may occur after walking only a few
short blocks or after walking up a slight incline. Any prolonged pressure on
the foot can cause pressure areas that become ulcerated, infected, and
gangrenous. The outcomes of arterial insufficiency in the elderly person
include reduced mobility and activity and a loss of independence.
Related Topics