Chapter: Medical Surgical Nursing: Vascular Disorders and Problems of Peripheral Circulation
Varicose Veins
VARICOSE
VEINS
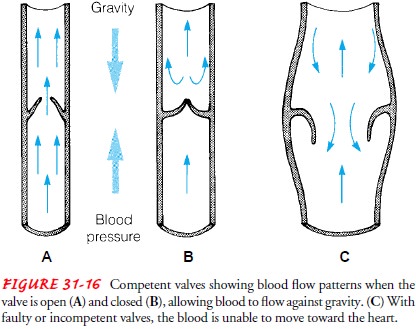
Varicose
veins (varicosities) are abnormally dilated, tortuous, superficial veins caused
by incompetent venous valves (see Fig. 31-16). Most commonly, this condition
occurs in the lower extremities, the saphenous veins, or the lower trunk;
however, it can occur elsewhere in the body, such as esophageal varices.
It is
estimated that varicose veins occur in up to 60% of the adult population in the
United States, with an increased inci-dence correlated with increased age (
Johnson, 1997). The condi-tion is most common in women and in people whose occupations
require prolonged standing, such as salespeople, hair stylists, teachers,
nurses, ancillary medical personnel, and construction workers. A hereditary
weakness of the vein wall may contribute to the de-velopment of varicosities,
and it is not uncommon to see this con-dition occur in several members of the
same family. Varicose veins are rare before puberty. Pregnancy may cause
varicosities. The leg veins dilate during pregnancy because of hormonal effects
related to distensibility, increased pressure by the gravid uterus, and
increased blood volume which all contribute to the develop-ment of varicose
veins ( Johnson, 1997).
Pathophysiology
Varicose
veins may be considered primary (without involvement of deep veins) or
secondary (resulting from obstruction of deep veins). A reflux of venous blood
in the veins results in venous stasis. If only the superficial veins are
affected, the person may have no symptoms but may be troubled by the appearance
of the dilated veins.
Clinical Manifestations
Symptoms,
if present, may take the form of dull aches, muscle cramps, and increased
muscle fatigue in the lower legs. Ankle edema and a feeling of heaviness of the
legs may occur. Nocturnal cramps are common. When deep venous obstruction
results in varicose veins, patients may develop the signs and symptoms of
chronic venous insufficiency: edema, pain, pigmentation, and ulcerations.
Susceptibility to injury and infection is increased.
Assessment and Diagnostic Findings
Diagnostic
tests for varicose veins include the duplex scan, which documents the anatomic
site of reflux and provides a quantitative measure of the severity of valvular
reflux. Air plethysmography measures the changes in venous blood volume.
Venography is not routinely performed to evaluate for valvular reflux. When it
is used, however, it involves injecting an x-ray contrast agent into the leg
veins so that the vein anatomy can be visualized by x-ray studies during
various leg movements.
Prevention
The
patient should avoid activities that cause venous stasis, such as wearing tight
socks or a constricting panty girdle, crossing the legs at the thighs, and
sitting or standing for long periods. Chang-ing position frequently, elevating
the legs when they are tired, and getting up to walk for several minutes of
every hour promote cir-culation. The patient should be encouraged to walk 1 or
2 miles each day if there are no contraindications. Walking up the stairs
rather than using the elevator or escalator is helpful in promoting
circulation. Swimming is also good exercise for the legs.
Elastic
compression stockings, especially knee-high stockings, are useful. Patients are
more likely to use knee-high stockings than thigh-high stockings. The
overweight patient should be encour-aged to begin a weight-reduction plan.
Medical Management
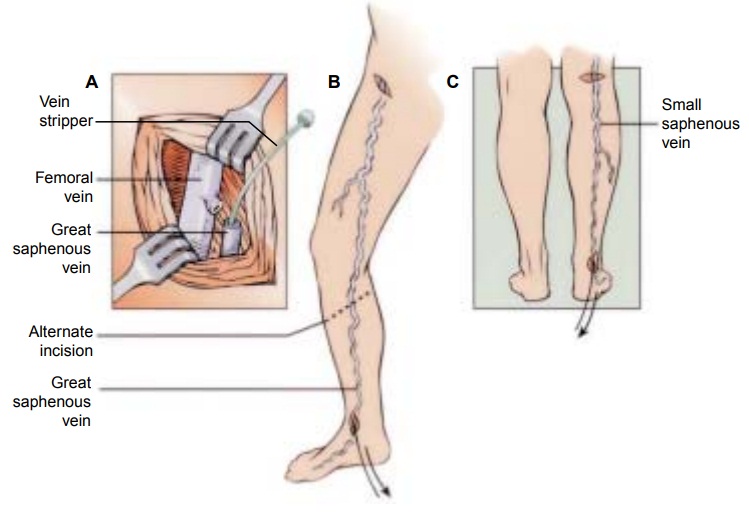
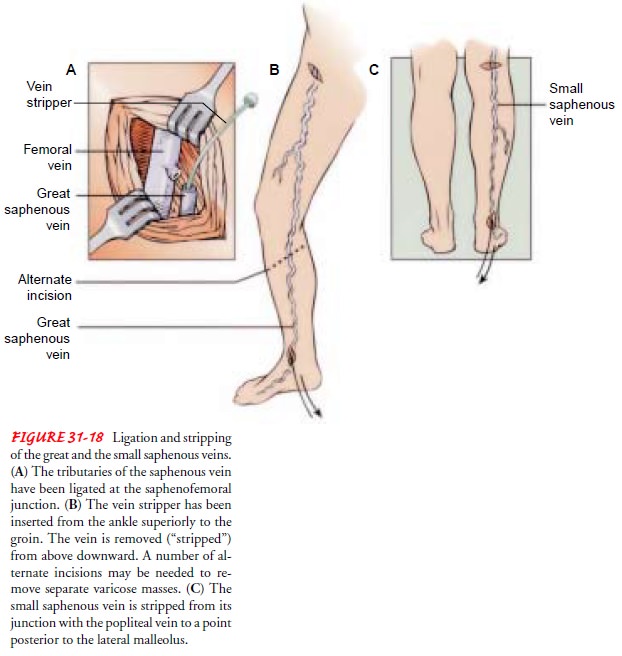
Surgery
for varicose veins requires that the deep veins be patent and functional. The
saphenous vein is ligated and divided. The vein is ligated high in the groin,
where the saphenous vein meets the femoral vein. Additionally, the vein may be
removed (stripped). After the vein is ligated, an incision is made in the
ankle, and a metal or plastic wire is passed the full length of the vein to the
point of ligation. The wire is then withdrawn, pulling (removing, “stripping”)
the vein as it is removed (Fig. 31-18). Pressure and elevation keep bleeding at
a minimum during surgery.
SCLEROTHERAPY
In
sclerotherapy, a chemical is injected into the vein, irritating the venous
endothelium and producing localized phlebitis and fibro-sis, thereby
obliterating the lumen of the vein. This treatment may be performed alone for
small varicosities or may follow vein ligation or stripping. Sclerosing is
palliative rather than curative. After the sclerosing agent is injected,
elastic compression ban-dages are applied to the leg and are worn for
approximately 5 days. The health care provider who performed sclerotherapy
removes the first bandages. Elastic compression stockings are then worn for an
additional 5 weeks.
After
sclerotherapy, patients are encouraged to perform walk-ing activities as
prescribed to maintain blood flow in the leg. Walking enhances dilution of the
sclerosing agent.
Nursing Management
Surgery
can be performed in an outpatient setting, or patients can be admitted to the
hospital on the day of surgery and discharged the next day, but nursing
measures are the same as if the patient were hospitalized. Bed rest is
maintained for 24 hours, after which the patient begins walking every 2 hours
for 5 to 10 min-utes. Elastic compression stockings are used to maintain
com-pression of the leg. They are worn continuously for about 1 week after vein
stripping. The nurse assists the patient to perform ex-ercises and move the
legs. The foot of the bed should be elevated. Standing still and sitting are
discouraged.
PROMOTING COMFORT AND UNDERSTANDING
Analgesics are prescribed to help patients move affected extremi-ties more comfortably. Dressings are inspected for bleeding, par-ticularly at the groin, where the risk of bleeding is greatest. The nurse is alert for reported sensations of “pins and needles.” Hyper sensitivity to touch in the involved extremity may indicate a tem-porary or permanent nerve injury resulting from surgery, because the saphenous vein and nerve are close to each other in the leg.
Usually,
the patient may shower after the first 24 hours. The patient is instructed to
dry the incisions well with a clean towel using a patting technique rather than
rubbing. Application of skin lotion is to be avoided until the incisions are
completely healed to decrease the chance of developing an infection.
If the
patient underwent sclerotherapy, a burning sensation in the injected leg may be
experienced for 1 or 2 days. The nurse may encourage the use of a mild
analgesic (eg, propoxyphene napsylate and acetaminophen [Darvocet N], oxycodone
and acetaminophen [Percocet], oxycodone and acetylsalicylic acid [Percodan]) as
pre-scribed by a physician or nurse practitioner and walking to pro-vide
relief.
PROMOTING HOME AND COMMUNITY-BASED CARE
Patients
require long-term elastic support of the leg after dis-charge, and plans are
made to obtain adequate supplies of elas-tic compression stockings or bandages
as appropriate. Exercises of the legs are necessary; the development of an
individualized plan requires consultation with the patient and the health care
team.
Related Topics