Chapter: Medical Surgical Nursing: Vascular Disorders and Problems of Peripheral Circulation
Nursing Process: The Patient Who Has Peripheral Arterial Insufficiency of the Extremities
NURSING
PROCESS:THE PATIENT WHO HAS PERIPHERAL ARTERIAL INSUFFICIENCY OF THE EXTREMITIES
Assessment
The
nursing assessment includes a complete health and medica-tion history and
identification of risk factors for peripheral artery disease. Signs and
symptoms detected during the nursing assess-ment may include claudication pain;
rest pain in the forefoot; pallor, rubor, or cyanosis; weak or absent
peripheral pulses; and skin breakdown or ulcerations.
Nursing Diagnosis
Based
on assessment data, major nursing diagnoses for the patient may include the
following:
· Ineffective peripheral
tissue perfusion related to compro-mised circulation
· Chronic pain related to
impaired ability of peripheral vessels to supply tissues with oxygen
· Risk for impaired skin
integrity related to compromised circulation
· Deficient knowledge
regarding self-care activities
Planning and Goals
The
major goals for the patient may include increased arterial blood supply to the
extremities, promotion of vasodilation, pre-vention of vascular compression,
relief of pain, attainment or main-tenance of tissue integrity, and adherence
to the self-care program.
Measures used by the patient and members of the health care team to accomplish a single goal must be evaluated in terms of the positive and the negative effects these measures may have on the simultaneous achievement of other goals. An overview of the care of a patient with peripheral arterial problems is provided in the Plan of Nursing Care: The Patient With Peripheral Vascular Problems.
Nursing Interventions
IMPROVING PERIPHERAL ARTERIAL CIRCULATION
Arterial
blood supply to a body part can be enhanced by position-ing the part below the
level of the heart. For the lower extremities, this is accomplished by
elevating the head of the patient’s bed on 15-cm (6-inch) blocks or by having
the patient use a reclining chair or sit with the feet resting on the floor.
The
nurse can assist the patient with walking or other moder-ate or graded
isometric exercises that may be prescribed to pro-mote blood flow and encourage
the development of collateral circulation. The nurse instructs the patient to
walk to the point of pain, rest until pain subsides, and then resume walking so
that en-durance can be increased as collateral circulation develops. Pain can
serve as a guide in determining the amount of exercise appro-priate for an
individual. The onset of pain indicates that the tis-sues are not receiving
adequate oxygen, signaling the patient to rest before continuing activity.
However, a regular exercise program can result in increased walking distance
before the onset of clau-dication. The amount of exercise a patient can
tolerate before the onset of pain is determined to provide a baseline for
evaluation.
Not
all patients with peripheral vascular disease should exercise. Before
recommending any exercise program, the primary health care provider should be
consulted. Conditions that worsen with ac-tivity include leg ulcers,
cellulitis, gangrene, or acute thrombotic occlusions.
PROMOTING VASODILATION AND PREVENTING VASCULAR COMPRESSION
Arterial
dilation promotes increased blood flow to the extremities and is therefore a
desirable goal for patients with peripheral arte-rial disease. However, if the
arteries are severely sclerosed, inelas-tic, or damaged, dilation is not
possible. For this reason, measures to promote vasodilation, such as
medications or surgery, may be only minimally effective.
Nursing
interventions may involve applications of warmth to promote arterial flow and
instructions to the patient to avoid ex-posure to cold temperatures, which
causes vasoconstriction. Adequate clothing and warm temperatures protect the
patient from chilling. If chilling occurs, a warm bath or drink is helpful.
When
heat is applied directly to ischemic extremities, the tem-perature of the heat
source must not exceed body temperature. Even at lower temperatures, burn
injuries can occur in ischemic extremities. Excess heat may increase the
metabolic rate of the ex-tremities and increase the need for oxygen beyond that
provided by the reduced arterial flow through the diseased artery.
Nicotine
causes vasospasm and can thereby dramatically re-duce circulation to the
extremities. Tobacco smoke also impairs transport and cellular use of oxygen
and increases blood viscosity. Patients with arterial insufficiency who use
tobacco (ie, smoke, chew) must be fully informed of the effects of nicotine on
circu-lation and encouraged to stop using tobacco.
Emotional
upsets stimulate the sympathetic nervous system, resulting in peripheral
vasoconstriction. Although emotional stress is unavoidable, it can be minimized
to some degree by avoiding stressful situations when possible or by
consistently fol-lowing a stress-management program. Counseling services or
re-laxation training may be indicated for people who cannot cope effectively
with situational stressors.
Constrictive
clothing and accessories such as tight socks, panty girdles, and shoelaces impede
circulation to the extremities and promote venous stasis and therefore should
be avoided. Cross-ing the legs should be discouraged because it compresses
vessels in the legs.
RELIEVING PAIN
Frequently, the pain associated with peripheral arterial insuffi-ciency is chronic and continuous. It limits activities, affects work and responsibilities, disturbs sleep, and alters patients’ sense of well-being. Patients are often depressed, irritable, and unable to exert the energy necessary to execute prescribed therapies, mak-ing pain relief even more difficult. Analgesics such as oxycodone plus acetylsalicylic acid (Percodan) or oxycodone plus acetamin ophen (Percocet) may be helpful in reducing pain to the point where the patient can participate in the therapies that can increase circulation and ultimately relieve pain more effectively.
MAINTAINING TISSUE INTEGRITY
Poorly
nourished tissues are susceptible to damage and infec-tion. When lesions develop,
healing may be delayed or inhib-ited because of the poor blood supply to the
area. Infected, nonhealing ulcerations of the extremities can be debilitating
and may require prolonged and often expensive treatments. Am-putation of an
ischemic limb may eventually be necessary. Mea-sures to prevent these
complications must be a high priority and vigorously implemented.
Trauma
to the extremities must be avoided. Advising the pa-tient to wear sturdy,
well-fitting shoes or slippers to prevent foot injury and blisters may be
helpful, as may be recommending neu-tral soaps and body lotions to prevent
drying and cracking of skin. Scratching and vigorous rubbing can abrade skin
and create a site for bacterial invasion; therefore, feet should be patted dry.
Stock-ings should be clean and dry. Fingernails and toenails should be
carefully trimmed straight across and sharp corners filed to follow the contour
of the nail. If nails are thick and brittle and cannot be trimmed safely, a
podiatrist must be consulted. Corns and calluses need to be removed by a health
care professional. Special shoe in-serts may be needed to prevent calluses from
recurring. All signs of blisters, ingrown toenails, infection, or other
problems should bereported to health care professionals for treatment and
follow-up. Patients with diminished vision may require assistance in
periodi-cally examining the lower extremities for trauma.
Good
nutrition promotes healing and prevents tissue break-down and is therefore
included in the overall therapeutic program for patients with peripheral
vascular disease. Eating a well-balanced diet that contains adequate protein
and vitamins is nec-essary for patients with arterial insufficiency. Key
nutrients play specific roles in wound healing. Vitamin C is essential for
colla-gen synthesis and capillary development. Vitamin A enhances
epithelialization. Zinc is necessary for cell mitosis and cell prolif-eration.
Obesity strains the heart, increases venous congestion, and reduces
circulation; therefore, a weight-reduction plan may be necessary for some
patients. A diet low in lipids may be indi-cated for patients with
atherosclerosis.
PROMOTING HOME AND COMMUNITY-BASED CARE
The
self-care program is planned with the patient so that activities that promote
arterial and venous circulation, relieve pain, and pro-mote tissue integrity
are acceptable. The patient and family are helped to understand the reasons for
each aspect of the program and the possible consequences of nonadherence.
Long-term care of the feet and legs is of prime importance in the prevention of
trauma, ulceration, and gangrene. The Plan of Nursing Care describes nurs-ing
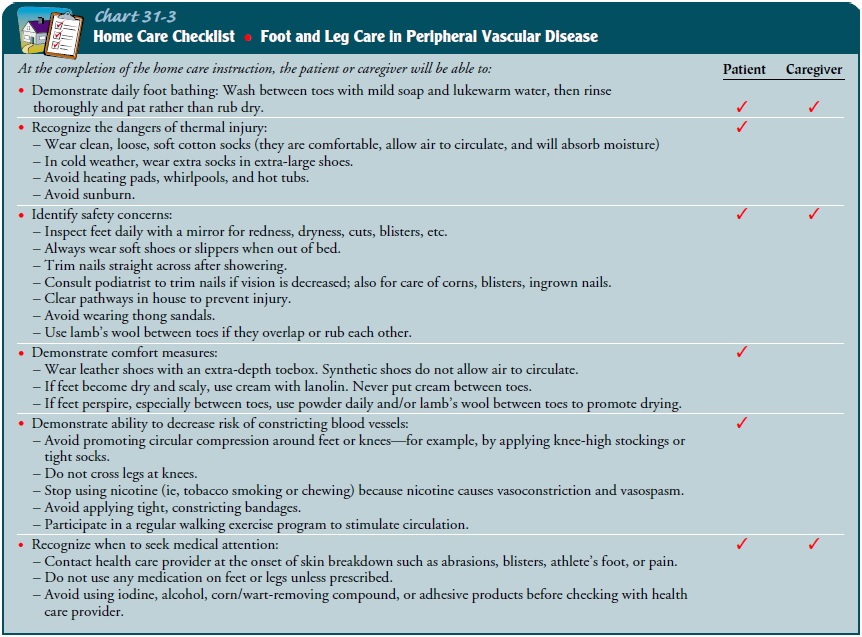
care for patients with peripheral vascular disease. Chart 31-3 provides
detailed patient instructions for foot and leg care.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1) Demonstrates an increase
in arterial blood supply to extremities
a)
Exhibits extremities warm to touch
b)
Has improved color of extremities (ie, free of
rubor or cyanosis)
c)
Experiences decreased muscle pain with exercise
d)
Demonstrates an increase in walking distance or
duration
2) Promotes vasodilation;
prevents vascular compression
a)
Protects extremities from exposure to cold
b)
Avoids use of tobacco
c) Uses stress management
strategies to minimize emo-tional upset
d)
Wears nonconstricting clothing
e)
Avoids leg crossing
f)
Takes medication as prescribed
3) Has decrease in severity
and duration of pain
4) Attains or maintains
tissue integrity
a)
Avoids trauma and irritation to skin
b)
Wears protective shoes
c)
Adheres to meticulous hygienic regimen
d)
Eats a healthy diet that contains adequate protein,
vita-mins A and C, and zinc
e)
Performs self-care activities
Related Topics