Chapter: Medical Surgical Nursing: Vascular Disorders and Problems of Peripheral Circulation
Aortic Aneurysm
AORTIC
ANEURYSM
An
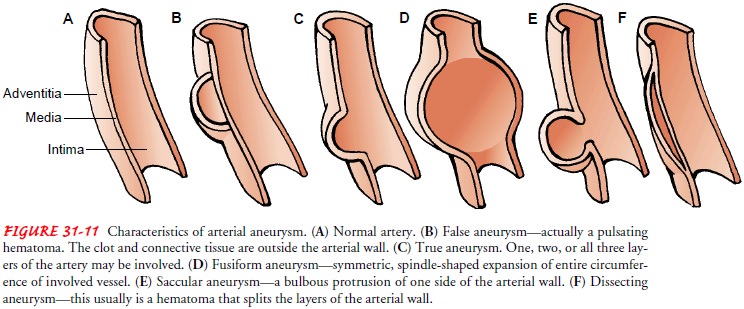
aneurysm is a localized sac or dilation formed at a weak point in the wall of
the aorta (Fig. 31-11). It may be classified by its shape or form. The most
common forms of aneurysms are sac-cular or fusiform. A saccular aneurysm
projects from one side of the vessel only. If an entire arterial segment
becomes dilated, a fusiform aneurysm develops. Very small aneurysms due to
local-ized infection are called mycotic aneurysms.
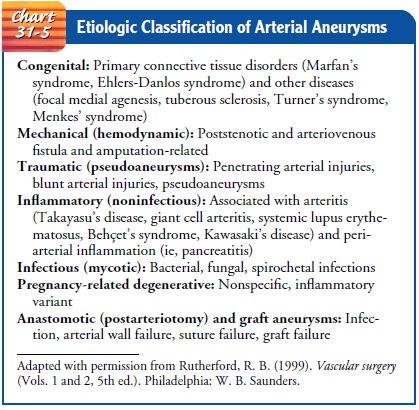
Historically,
the cause of abdominal aortic aneurysm, the most common type of degenerative
aneurysm, has been attributed to atherosclerotic changes in the aorta. Other
causes of aneurysm formation are listed in Chart 31-5. Aneurysms are serious
because they can rupture, leading to hemorrhage and death.
THORACIC AORTIC ANEURYSM
Approximately
85% of all cases of thoracic aortic aneurysm are caused by atherosclerosis.
They occur most frequently in men between the ages 40 and 70 years. The
thoracic area is the most common site for a dissecting aneurysm. About one
third of pa-tients with thoracic aneurysms die of rupture of the aneurysm
(Rutherford, 1999).
Clinical Manifestations
Symptoms are variable and depend on how rapidly the aneurysm dilates and how the pulsating mass affects surrounding intratho-racic structures. Some patients are asymptomatic. In most cases, pain is the most prominent symptom. The pain is usually con-stant and boring but may occur only when the person is supine.
Other
conspicuous symptoms are dyspnea, the result of pressure of the sac against the
trachea, a main bronchus, or the lung itself; cough, frequently paroxysmal and
with a brassy quality; hoarseness, stridor, or weakness or complete loss of the
voice (aphonia), re-sulting from pressure against the left recurrent laryngeal
nerve; and dysphagia (difficulty in swallowing) due to impingement on the
esophagus by the aneurysm.
Assessment and Diagnostic Findings
When
large veins in the chest are compressed by the aneurysm, the superficial veins
of the chest, neck, or arms become dilated, and edematous areas on the chest
wall and cyanosis are often evident. Pressure against the cervical sympathetic
chain can result in unequal pupils. Diagnosis of a thoracic aortic aneurysm is
prin-cipally made by chest x-ray, transesophageal echocardiography, and CT.
Medical Management
In
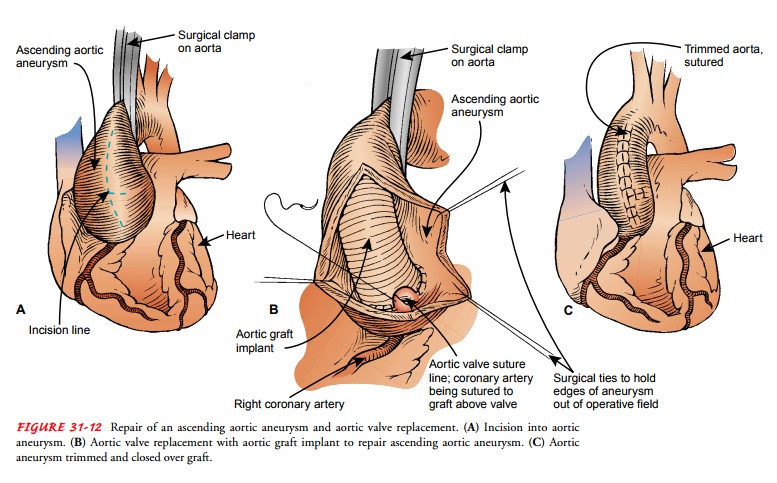
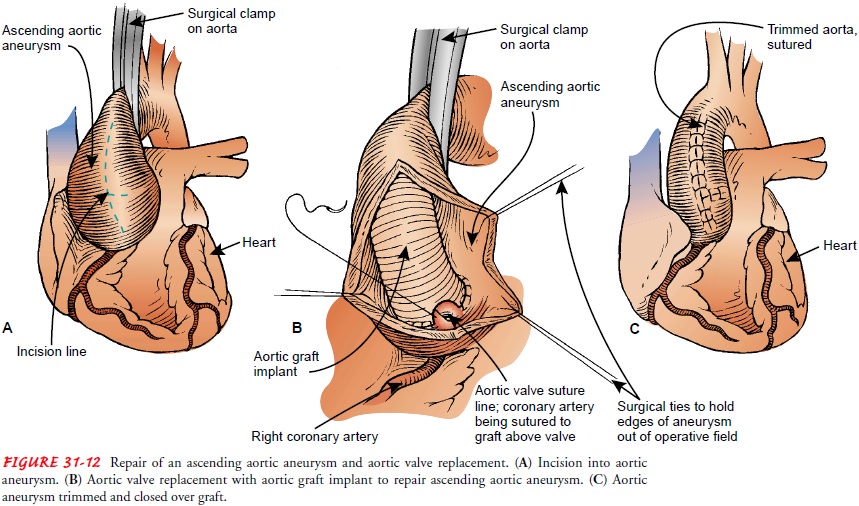
most cases, an aneurysm is treated by surgical repair. General measures such as
controlling blood pressure and correcting risk factors may be helpful. It is
important to control blood pressure in patients with dissecting aneurysms.
Systolic pressure is main-tained at about 100 to 120 mm Hg with
antihypertensive med-ications (eg, hydralazine hydrochloride [Hydralazine],
esmolol hydrochloride [Brevibloc] or another beta-blocker such as atenolol
[Tenormin] or timolol maleate [Timoptic]). Pulsatile flow is re-duced by
medications that reduce cardiac contractility (eg, propranolol [Inderal]). The
goal of surgery is to repair the aneurysm and restore vascular continuity with
a vascular graft (Fig. 31-12). Intensive monitoring is usually required after
this type of surgery, and the patient is cared for in the critical care unit.
Repair of thoracic aneurysms using endovascular grafts implanted (de-ployed) percutaneously
in an interventional laboratory (eg, cardiac catheterization laboratory) may
decrease postoperative recovery time and decrease complications compared with
traditional sur-gical techniques.
ABDOMINAL AORTIC ANEURYSM
The
most common cause of abdominal aortic aneurysm is athero-sclerosis. The
condition, which is more common among Cau-casians, affects men four times more
often than women and is most prevalent in elderly patients (Rutherford, 1999).
Most of these aneurysms occur below the renal arteries (infrarenal aneurysms).
Untreated, the eventual outcome may be rupture and death.
Pathophysiology
All aneurysms involve a damaged media layer of the vessel. This may be caused by congenital weakness, trauma, or disease. After an aneurysm develops, it tends to enlarge. Risk factors include ge-netic predisposition, smoking (or other tobacco use), and hyper-tension; more than one half of patients with aneurysms have hypertension.
Clinical Manifestations
About
two fifths of patients with abdominal aortic aneurysms have symptoms; the
remainder do not. Some patients complain that they can feel their heart beating
in their abdomen when lying down, or they may say they feel an abdominal mass
or abdomi-nal throbbing. If the abdominal aortic aneurysm is associated with
thrombus, a major vessel may be occluded or smaller distal occlusions may
result from emboli. A small cholesterol, platelet, or fibrin emboli may lodge
in the interosseous or digital arteries, causing blue toes.
Assessment and Diagnostic Findings
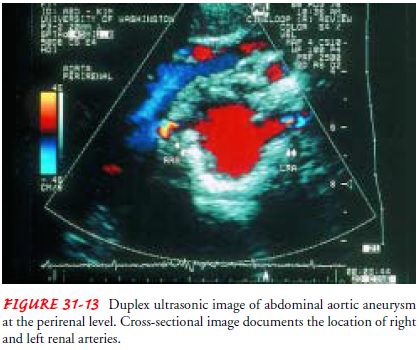
The
most important diagnostic indication of an abdominal aortic aneurysm is a
pulsatile mass in the middle and upper abdomen. About 80% of these aneurysms
can be palpated. A systolic bruit may be heard over the mass. Duplex
ultrasonography or CT is used to determine the size, length, and location of
the aneurysm (Fig. 31-13). When the aneurysm is small, ultrasonography is
conducted at 6-month intervals until the aneurysm reaches a size at which
surgery to prevent rupture is of more benefit than the possible complications
of a surgical procedure. Some aneurysms remain stable over many years of
observation.
Gerontologic Considerations
Most
abdominal aneurysms occur in patients between the ages of 60 and 90 years. Rupture
is likely with coexisting hypertension and with aneurysms wider than 6 cm. In
most cases at this point, the chances of rupture are greater than the chance of
death during surgical repair. If the elderly patient is considered at moderate
risk for complications related to surgery or anesthesia, the aneurysm is not
repaired until it is at least 5 cm (2 inches) wide.
Medical Management
An
expanding or enlarging abdominal aneurysm is likely to rupture. Surgery is the
treatment of choice for abdominal aneurysms wider than 5 cm (2 inches) wide or
those that are enlarging.
SURGICAL MANAGEMENT
The standard treatment for abdominal aortic aneurysm repair has been open surgical repair of the aneurysm by resecting the vessel and sewing
a bypass graft in place. The mortality rate associated with elective aneurysm
repair, a major surgical procedure, is re-ported to be 1% to 4%. The prognosis
for a patient with a rup-tured aneurysm is poor, and surgery is performed
immediately (Rutherford, 1999).
An
alternative for treating an infrarenal abdominal aortic aneu-rysm is
endovascular grafting. Endovascular grafting involves the transluminal
placement and attachment of a sutureless aortic graft prosthesis across an
aneurysm (Fig. 31-14). This procedure can be performed under local or regional
anesthesia. Endovascular graft-ing of abdominal aortic aneurysms may be
performed if the patient’s abdominal aorta and iliac arteries are not extremely
tor-tuous and if the aneurysm does not begin at the level of the renal
arteries. Clinical trials are evaluating endograft treatment of ab-dominal
aortic aneurysms at or above the level of the renal arteries and the thoracic
aorta. Potential complications include bleeding, hematoma, or wound infection at
the femoral insertion site; distal ischemia or embolization; dissection or
perforation of the aorta; graft thrombosis; graft infection; break of the
attachment system; graft migration; proximal or distal graft leaks; delayed
rupture; and bowel ischemia.
Nursing Management
Before
surgery, nursing assessment is guided by anticipating a rupture and by
recognizing that the patient may have cardiovas-cular, cerebral, pulmonary, and
renal impairment from athero-sclerosis. The functional capacity of all organ systems
should be assessed. Medical therapies designed to stabilize physiologic
func-tion should be promptly implemented.
Signs
of impending rupture include severe back pain or ab-dominal pain, which may be
persistent or intermittent and is oftenlocalized in the middle or lower abdomen
to the left of the midline. Low back pain may also be present because of
pressure of the aneurysm on the lumbar nerves. This is a serious symptom,
usually indicating that the aneurysm is expanding rapidly and is about to rupture.
Indications of a rupturing abdominal aortic aneurysm in-clude constant, intense
back pain; falling blood pressure; and de-creasing hematocrit. Rupture into the
peritoneal cavity is rapidly fatal. A retroperitoneal rupture of an aneurysm
may result in hematomas in the scrotum, perineum, flank, or penis. Signs of
heart failure or a loud bruit may suggest a rupture into the vena cava. Rupture
into the vena cava results in the higher-pressure ar-terial blood entering the
lower-pressure venous system and causing turbulence, which is heard as a bruit.
The high blood pressure and increased blood volume returning to the right heart
from the vena cava may cause the right heart to fail. The overall surgical
mortal-ity rate associated with a ruptured aneurysm is 50% to 75%.
Postoperative
care requires intense monitoring of pulmonary, cardiovascular, renal, and
neurologic status. Possible complica-tions of surgery include arterial
occlusion, hemorrhage, infection, ischemic bowel, renal failure, and impotence.
Related Topics