Chapter: Medical Surgical Nursing: Emergency Nursing
Wounds - Emergency Nursing
Wounds
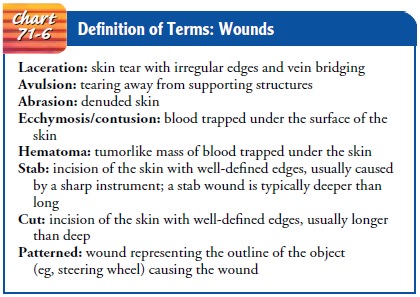
Wounds involving injury to soft tissues can vary from minor tears to severe crushing injuries. The types of wounds that may occur are defined in Chart 71-6. The primary goal is to restore the phys-ical integrity and function of the injured tissue, with minimal scarring and without infection. Proper documentation of the wound, using precise descriptions and correct terminology, is essential. Such information may be needed in the future for forensic evidence. Photographs are helpful because they provide an accurate, visible description of the wound.
Determining when and how the wound occurred is important, because a treatment delay
exceeding 3 hours increases infection risk. Using aseptic technique, the
clinician inspects the wound to determine the extent of damage to underlying
structures. Sen-sory, motor, and vascular function are evaluated for changes
that might indicate complications.
Management
WOUND CLEANSING
Hair around the wound
may be clipped or shaved (only as di-rected) if it is anticipated that the
hairs will interfere with wound closure. Typically, the area around the wound
is cleaned with normal saline solution or a polymer agent (eg, SureClens).
Anti-bacterial agents, such as povidone-iodine (Betadine) or hydrogen peroxide,
should not be allowed to get deep into the wound with-out thorough rinsing.
These agents are used only for the initial cleansing because they injure
exposed and healthy tissue, resulting in further cell injury.
If indicated, the area
is infiltrated with a local intradermal anes-thetic through the wound margins
or by regional block. Patients with soft tissue injuries usually have localized
pain at the site of injury. The nurse then assists the physician, nurse
practitioner, or physician’s assistant in cleaning and débriding the wound.
The wound is irrigated
gently and copiously with sterile iso-tonic saline solution to remove surface
dirt. Devitalized tissue and foreign matter are removed because they impede
healing and may encourage infection. Any small bleeding vessels are clamped or
tied. Alternatively, hemostasis may be achieved with cauteri-zation. After
wound treatment, a nonadherent dressing is com-monly applied to protect the
wound. The dressing may serve as a splint and also as a reminder to the patient
that the area is injured.
PRIMARY CLOSURE
The decision to suture a
wound depends on the nature of the wound, the time since the injury was
sustained, the degree of con-tamination, and the vascularity of tissues. If
primary closure is in-dicated, the wound is sutured, usually by the physician,
with the patient receiving a form of anesthesia known as moderate sedation.
Wound closure begins when subcutaneous fat is brought together loosely with a
few sutures to close off the dead space. The sub-cuticular layer is then
closed, and finally the epidermis is closed. Sutures are placed near the wound
edge, with the skin edges leveled carefully to promote optimal healing. Instead
of sutures, sterile strips of reinforced microporous tape or a bonding agent
(skin glue) may be used to close clean, superficial wounds.
DELAYED PRIMARY CLOSURE
Delayed primary closure may be indicated if tissue has
been lost or there is a high potential for infection.
A thin layer of gauze (to ensure drainage and prevent
pooling of exudate), covered by an occlusive dressing, may be used. Other
options include split-thickness cadaver or porcine xenografts to simulate the
function of epithelium. The wound is splinted in a functional position to
prevent motion and decrease the possibility of contracture.
If there are no signs of suppuration, the wound may be
su-tured (with the patient receiving a local anesthetic). Use of anti-biotics
to prevent infection depends on factors such as how the injury occurred, the
age of the wound, and the risk for contami-nation. The site is immobilized and
elevated to limit accumula-tion of fluid in the interstitial spaces of the
wound.
Tetanus prophylaxis is administered as prescribed, based
on the condition of the wound and the patient’s immunization status. The
patient is instructed about signs and symptoms of in-fection and is told to
contact the health care provider or clinic if there is sudden or persistent
pain, fever or chills, bleeding, rapid swelling, foul odor, drainage, or
redness surrounding the wound.
Related Topics