Chapter: Medical Surgical Nursing: Emergency Nursing
Airway Obstruction - Emergency Nursing
Airway
Obstruction
Acute upper airway
obstruction is a life-threatening medical emergency. The airway may be
partially or completely occluded. If the airway is completely obstructed,
permanent brain damage or death will occur within 3 to 5 minutes secondary to
hypoxia. Partial obstruction of the airway can lead to progressive hypoxia,
hypercarbia, and respiratory and cardiac arrest.
Pathophysiology
Upper airway obstruction
has a number of causes, including as-piration of foreign bodies, anaphylaxis,
viral or bacterial infection, trauma, and inhalation or chemical burns. In adults,
aspiration of a bolus of meat is the most common cause of airway obstruc-tion.
In children, small toys, buttons, coins, and other objects are commonly
aspirated in addition to food. Peritonsillar abscesses, epiglottitis, and other
acute infectious processes of the posterior pharynx can result in airway
obstruction.
Clinical Manifestations
Common signs and
symptoms include choking, apprehensive ap-pearance, inspiratory and expiratory
stridor, labored breathing, use of accessory muscles (suprasternal and
intercostal retraction), flaring nostrils, increasing anxiety, restlessness,
and confusion. Cyanosis and loss of consciousness develop as hypoxia worsens.
Assessment and Diagnostic Findings
Assessment of the patient who has a foreign object
occluding the airway may involve simply asking the person whether he or she is
choking and requires help. If the person is unconscious, inspec-tion of the
oropharynx may reveal the offending object. X-rays, laryngoscopy, or
bronchoscopy also may be performed.
Gerontologic Considerations
For elderly patients,
especially those in extended care facilities, sedatives and hypnotic
medications, diseases affecting motor co-ordination (eg, Parkinson’s disease),
and mental dysfunction (eg, dementia, mental retardation) are risk factors for
asphyxia-tion by food. Nursing staff involved in the care of elderly patients
must be aware of the symptoms of upper airway obstruction and be skillful in
performing the Heimlich maneuver. Typically, the victim with a foreign body
airway obstruction cannot speak, breathe, or cough. The patient may clutch the
neck between the thumb and fingers (universal distress signal ). The first
response is to ask this person whether he or she is choking.
If the patient can
breathe and cough spontaneously, a partial obstruction should be suspected. The
victim is encouraged to cough forcefully and to persist with spontaneous
coughing and breathing efforts as long as good air exchange exists. There may
be some wheezing between coughs. If the patient demonstrates a weak,
ineffective cough, high-pitched noise while inhaling, in-creased respiratory
difficulty, or cyanosis, the patient should be managed as if there were
complete airway obstruction.
After the obstruction is removed, rescue breathing is
initiated. If the patient has no pulse, cardiac compressions are instituted.
These measures provide oxygen to the brain, heart, and other vital organs until
definitive medical treatment can restore and support normal heart and
ventilatory activity.
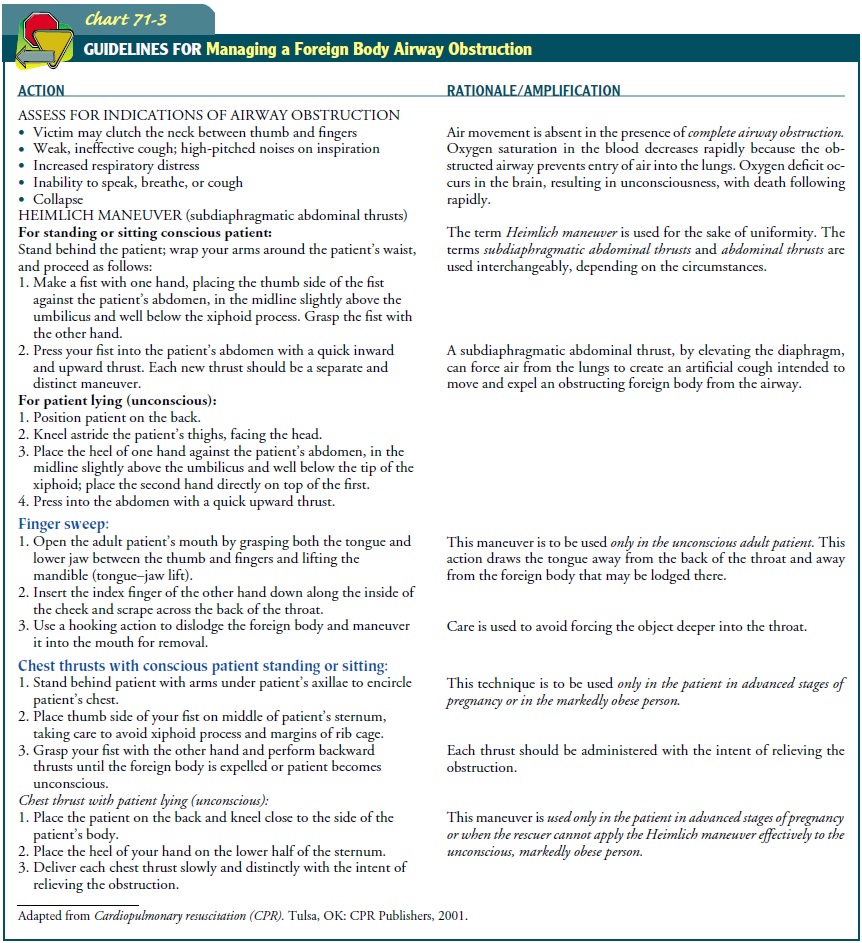
Management
Establishing an airway
may be as simple as repositioning the pa-tient’s head to prevent the tongue
from obstructing the pharynx. Alternatively, other maneuvers, such as abdominal
thrusts, the head-tilt–chin-lift maneuver, the jaw-thrust maneuver, or
inser-tion of specialized equipment may be needed to open the airway, remove a
foreign body, or maintain the airway (Chart 71-3). In all maneuvers, the
cervical spine must be protected from injury.
HEAD-TILT–CHIN-LIFT MANEUVER
The patient is placed
supine on a firm, flat surface. If the patient is lying face down, the body is
turned as a unit so that the head, shoulders, and torso move simultaneously
with no twisting. Next, the airway is opened using either the
head-tilt–chin-lift maneu-ver or the jaw-thrust maneuver. In the
head-tilt–chin-lift ma-neuver, one hand is placed on the victim’s forehead, and
firm backward pressure is applied with the palm to tilt the head back. The
fingers of the other hand are placed under the bony part of the lower jaw near
the chin and lifted up. The chin and the teeth are brought forward almost to
occlusion to support the jaw.
JAW-THRUST MANEUVER
After one hand is placed on each side of the patient’s
jaw, the an-gles of the victim’s lower jaw are grasped and lifted, displacing
the mandible forward. This is a safe approach to opening the airway of a victim
with suspected neck injury because it can be accom-plished without extending
the neck.
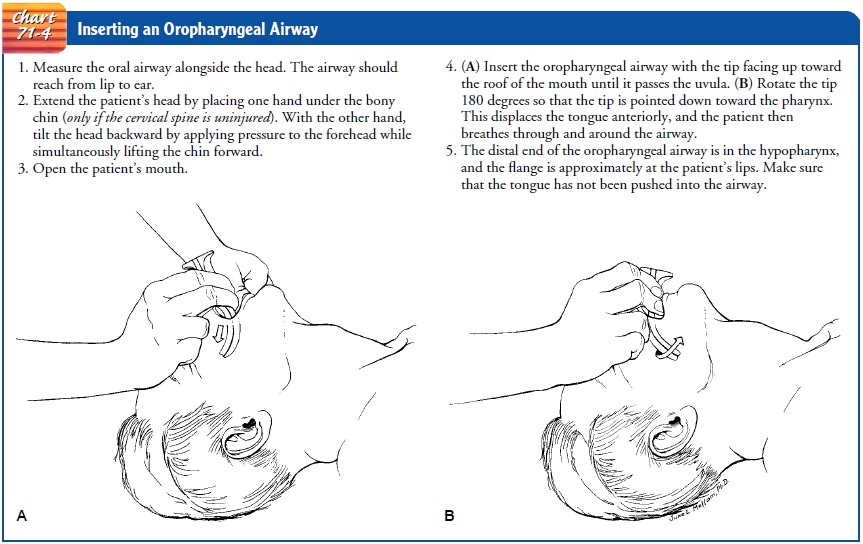
OROPHARYNGEAL AIRWAY INSERTION
An oropharyngeal airway is a semicircular tube or
tubelike plas-tic device that is inserted over the back of the tongue into the
lower posterior pharynx in a patient who is breathing sponta-neously but
unconscious (Chart 71-4). This type of airway prevents the tongue from falling
back against the posterior pharynx and obstructing the airway. It also allows
health care providers to suction secretions.
ENDOTRACHEAL INTUBATION
The purpose of
endotracheal intubation is to establish and main-tain the airway in patients
with respiratory insufficiency or hy-poxia. Endotracheal intubation is
indicated for the following reasons: (1) to establish an airway for patients
who cannot be ad-equately ventilated with an oropharyngeal airway, (2) to
bypass an upper airway obstruction, (3) to prevent aspiration, (4) to per-mit
connection of the patient to a resuscitation bag or mechanical ventilator, and
(5) to facilitate the removal of tracheobronchial secretions (Fig. 71-1).
Because the procedure requires skill, en-dotracheal intubation is performed
only by those who have had extensive training. These include physicians, nurse
anesthetists, respiratory therapists, flight nurses, and nurse practitioners.
The emergency nurse, however, is commonly called upon to assist with
intubation.
ALTERNATIVE INTUBATION METHOD
If the patient is outside the hospital and cannot be
intubated in the field, the emergency medical personnel may insert a
Com-bitube. The tube rapidly provides pharyngeal ventilation. When the tube is
inserted into the trachea, it functions like an endotra-cheal tube.
One of the two balloons
around the tube can be inflated. One balloon is large (100 mL) and occludes the
oropharynx. This could effectively provide for ventilation through forced air
by way of the larynx. The smaller balloon is inflated with 15 mL of air and can
effectively occlude the trachea if placed there. Breath sounds are auscultated
to make sure that the oropharyngeal cuff does not obstruct the glottis.
Patients can be ventilated through either port of the tube, depending on its
placement.
CRICOTHYROIDOTOMY (CRICOTHYROID MEMBRANE PUNCTURE)
Cricothyroidotomy is the opening of the cricothyroid mem-brane to establish
an airway. This procedure is used in emergency situations in which endotracheal
intubation is either not possible or contraindicated, as in airway obstruction
from extensive maxillo-facial trauma, cervical spine injuries, laryngospasm,
laryngeal edema (after an allergic reaction), hemorrhage into neck tissue, or
obstruction of the larynx.
After these maneuvers are performed, the patient is
assessed for breathing by watching for chest movement and listening and feeling
for air movement.
In such a case, nursing diagnoses would include
ineffective air-way clearance due to obstruction of the tongue, object, or
fluids (blood, saliva). The nursing diagnosis may also be ineffective breathing
pattern due to obstruction or injury.
Related Topics